.png?width=459&name=Add%20a%20heading%20(7).png)
No matter where you are or what you’re doing, you’re always being exposed to disease-causing pathogens. And while this may seem like a scary concept, you'll be happy to know that your immune system is working around the clock to fight off this bacteria and keep your body healthy. At least, that’s what it’s supposed to do…
Immunodeficiency, also called immune deficiency, is a state in which the body’s ability to fight infectious disease is compromised. Primary immune deficiency is one that’s inherited through genetic mutations while secondary, or acquired immune deficiency is one that’s caused by environmental factors, i.e., bacteria, viruses, or immunosuppressive drugs like cigarettes.
Recently, researchers have focused their sights on understanding the effect of chronic obstructive pulmonary disease (COPD) and other respiratory conditions on the immune system and what role the immune system plays in causing COPD. While COPD is not classified as an autoimmune disease (a disease that causes the immune system to attack the body), it’s still linked to the immune system in a number of ways. According to a study published in the American Thoracic Journal, COPD patients are more prone to respiratory infection and they’re less likely to recover from it than those without the disease.
While the correlation between immune deficiency and COPD is complex, it’s important for you to understand because it has a profound effect on your health and wellbeing. For most people, getting sick is just a part of life. However, for someone with COPD, getting sick could mean being at a higher risk for life-threatening exacerbations.
In the following sections, we’ll discuss how the immune system works, the various types of immune disorders, and most importantly, where COPD fits into all of this. Your pulmonologist and primary physician should be your first line of contact when it comes to improving and maintaining your immune system, so be sure to reach out to him/her if you have any questions or concerns.
How Does the Immune System Work?
Just like the name suggests, the ‘immune system’ isn’t one specific entity; it’s a whole host of processes that occur throughout the body that work in tandem to protect you from disease-causing microorganisms. In a healthy person, these processes are all running at full force and working together effectively as the body’s first line of defense.
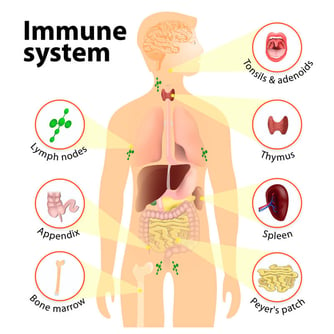
The immune system is one of the most complex parts of the body because it’s made up of a variety of different organs, cells, and proteins. There are three main tasks that the immune system is responsible for in the body:
- Recognizing harmful substances in your environment and keeping them out of the body.
- Neutralizing harmful pathogens inside the body such as parasites, fungi, viruses, and bacteria, then removing them.
- Fighting cancerous cells in the body.
Innate Immune System
All immune responses in the body can be divided into one of two different categories: innate or adaptive. The first of which, innate, is characterized by the body’s natural ability to fight harmful substances. Most of the components that make up you innate immune system are present at birth, but they can still develop and adapt over time.
Physical Barriers
While you may not think of your skin, eye lashes, and nose hair as part of the immune system, all of these are considered “physical barriers” and keep harmful substances from entering the body. The skin, for example, has a very low permeability, meaning it’s difficult for foreign substances to enter the body through it. However, other parts of the body like the mouth, nose, ears and eyes are open entry points to the rest of the body, this is why they need extra layers of immune protection.
Defense Mechanisms
Other innate immune responses in the body include things like saliva, mucous, tears, sweat, and secretions. Saliva, for example, plays an important role in managing bacteria in the mouth that causes gum disease. You may simply think of saliva as “water,” which is mostly what it is. However, saliva also contains a number of other substances like electrolytes, mucus, antibacterial compounds and various enzymes, all of which play a number of roles in protecting your oral health.

One important thing to note about your body’s natural defense mechanisms is that there’s a balance to all of it. When your body produces the ideal amount of saliva, mucous, tears, and sweat, you feel good. However, if something alters these processes, the defense mechanisms may be working against you. For example, smoking cigarettes results in high mucus production in the body. While mucus typically helps the body, too much of it can lead to airway obstruction and difficulty breathing.
Another way smoking affects the innate immune system is through the destruction of cilia. Cilia are tiny hair-like protuberances found in the lungs and wave back and forth to keep mucus and other substances out of the lungs. Smoking temporarily disables cilia, and long-term smoking can damage them meaning you’ll be more likely to get sick or experience difficulty breathing.
Inflammation
Inflammation is another key component of the innate immune response. Think of inflammation as a sort of signal that something is wrong. If you get an injury or an infection, inflammation occurs and white blood cells are sent to deal with the issue. Inflammation is a normal reactionary process for your body, but when it goes on for too long it may result in a chronic illness. What’s more, if inflammation never occurs, a seemingly harmless infection could become much more serious.
Adaptive Immune System
The adaptive immune system is your body’s ability to evolve and adjust based on its circumstances. Whenever you contract a disease, your adaptive immune system “remembers” it, making it much easier to fight off the next time it’s exposed to it. Unlike the innate immune system which reacts to general threats in the body, the adaptive immune system is activated when it’s exposed to pathogens. The adaptive immune system is also a lot slower to react than the innate immune system.

Self vs Non-Self Antigens
In order for the immune system to work effectively, it first needs to be able to differentiate between self and non-self substances, organs, and cells. Self-antigens are ones that originate in the body and should not be attacked while non-self antigens are foreign and can often cause harm to the body if they aren’t neutralized.
Your immune system is largely coordinated by white blood cells called lymphocytes. When these cells come across a non-self antigen in the blood, they produce something called an antibody that allows them to detect and bind to the antigen. After binding to the antigen, the antibody engulfs and digests it with macrophages through a process called phagocytosis.

If the body has encountered a substance before, it may have stored “memory” cells that remember the microbe, allowing it to create an antibody more quickly. This is why people are less likely to contract a disease if they’ve already had it, because their immune system is better equipped to fight it off before it becomes a problem. However, an antibody that recognizes one antigen will not be able to recognize another.
 Types of White Blood Cells
Types of White Blood Cells
Lymphocytes
There are three different types of lymphocytes: T cells, B cells, and natural killer cells. T cells got their name because they’re produced in the thymus gland, a pinkish-gray organ in between the lungs. T cells are able to recognize foreign bodies and attach to them while ignoring self antigens.
B cells, produced in bone marrow, are another important type of lymphocyte. These cells have a protein on them called the B-cell receptor which generates the antibodies necessary to neutralize an antigen. B cells are part of the adaptive immune system because they develop when they’re introduced to a foreign substance.
NK cells, or natural killer cells, are the third type of lymphocyte. They got the name “natural” killers because they are part of the innate immune system. While T and B cells need to be primed by antigen presenting cells, NK cells have natural immune capabilities. NK cells are known for fighting cells that show early signs of cancer as well as virally infected cells.
Monocytes
Monocytes are the largest type of white blood cell. They’re produced in bone marrow like many leukocytes and become a macrophage when it travels to different tissues of the body via the bloodstream. These cells ingest foreign material, kill microorganisms, and remove dead cells.
Granulocytes
Basophils
Basophils are a type of white blood cell referred to as granulocytes. A granulocyte white blood cell secretes substances called granules that play an important role in the immune system. When basophils are exposed to an allergen, they release a compound called histamine that causes dilation of capillaries and the contraction of smooth muscles.
Neutrophils
Neutrophils are usually the first white blood cells to arrive at the sight of infection because there are more of them than any other type of immune cell. Neutrophils neutralize bacterial infections through either phagocytosis or endocytosis.
Eosinophils
These are proinflammatory cells that contain two different lobes and a cytoplasm that contains up to 200 granules. These granules contain proteins and enzymes that are needed to destroy foreign substances. While eosinophils play similar roles to other white blood cells, they also have a physiological role in the formation of organs such as the postgestational mammary gland.
Humoral vs. Cellular Immunity
Humoral and cellular immunity are the two main mechanisms within adaptive immunity. Humoral comes from the Latin word “humor” meaning “fluid” or “moisture.” So, humoral immunity refers to immune responses occurring within the body’s fluids, especially the blood. In humoral immunity, the antibody will destroy viruses through either immune cytolysis or phagocytosis.

Unlike humoral immunity, cellular immunity does not use antibodies. Instead, phagocytes, antigen-specific cytotoxic T-lymphocytes, and cytokines are released in response to antigens. When there is a viral infection, cell-mediated immunity can help prevent it from spreading but also results in an inflammatory response which can damage vital tissues surrounding the virus, resulting in chronic disease.

Autoimmune Disease
An autoimmune disease is one that causes the immune system to be overactive and attack the body's tissues rather than pathogens or cancerous cells. Some autoimmune disease you may recognize include rheumatoid arthritis, multiple sclerosis, psoriasis, and vasculitis. There are more than 80 types of autoimmune disease, so it can be difficult to diagnose and differentiate each one.

Because autoimmune diseases cause increased immune system activity, they're often characterized by inflammation in the body. When treating these diseases, the goal is usually to reduce inflammation and reduce immune system activity. Your doctor may prescribe corticosteroids or other steroids that can help with this.
COPD and The Immune System
You may recall from earlier that inflammation is one of the key functions of the innate immune system. When cigarette smoke or other airborne irritants enter the lungs, structural and inflammatory cells in the lung begin to release proinflammatory mediators. These mediators create an inflammatory microenvironment that damages the lungs and leaves the immune system in a state of disrepair. Many researchers have found that this lung state leads to more frequent and severe respiratory infection as well as a host of problems throughout the body.

While most medical professionals don’t label COPD as an autoimmune disease, most acknowledge that it has autoimmune components. Think of inflammation as a catalyst for adverse side-effects throughout the body. Because your immune system is preoccupied with chronic inflammation in the lungs, it has fewer resources to use in other areas of the body that may need it.
Immune Dysfunction and COPD are a Two-Way Street
Another important thing to note about COPD and the immune system is that they’re a two-way street. In other words, a compromised immune system will lead to increased COPD symptoms, and COPD symptoms will lead to a compromised immune system. Like we mentioned before, smoking is the primary cause of COPD making up about 90 percent of COPD patients. Continuing to smoke with COPD will not only increase inflammation in the lungs, it will also weaken both your innate and adaptive immune system.

On the other hand, you should remember that only a small percentage of people who smoke actually develop emphysema or chronic bronchitis. This means that there are other factors at play in determining whether a smoker or someone exposed to lung irritants develops COPD. Researchers have found that both genetic makeup and the immune system play a role in determining whether someone develops the disease.
Mucus Hypersecretion
Mucus is a substance created by mucosal glands lining the nasal passages. Its function is to lubricate, moisten, and filter debris that enters the airway, preventing it from reaching the lungs. But mucus isn’t the only substance secreted in the upper body. There are also fluids created by cell membranes in the nose and sinuses. When you get sick or your immune system is compromised by something like smoking or seasonal allergies, these substances are thrown off balance. This means you may experience thicker mucus in the airways making it much more difficult to breathe.
Damaged Cilia
Unfortunately, many of the same things that cause COPD simultaneously damage your immune system. Cilia, tiny hair-like protrusions in the airways are one of the innate immune functions of the body that’s affected by cigarette smoking and air pollution. Much like mucus, cilia are part of a large ecosystem in your body that’s designed to prevent infection. While people who have never smoked or been exposed to a significant amount of pollution may have healthy cilia, most people who have COPD already have damaged cilia.

Another function of the cilia is to remove mucus and other substances from the airways. So, when the airways are inflamed due to bronchitis or the cilia are damaged and aren’t able to flow freely, congestion symptoms are likely going to stick around longer in someone with COPD and they may be more severe. This is one of the things that trigger a seemingly never ending cycle of sickness in people with chronic bronchitis and emphysema.
Overactive Immune System
If you’ve ever heard the term “progressive disease,” you may have wondered exactly what that means. What this means is that the disease can’t be cured or reversed. While COPD is a progressive disease, it is still very treatable, meaning symptoms can be reduced and you are able to slow the progression of inflammation in the lungs.
Normally, you think of the immune system as something that protects your body from infection and harm. However, when you have COPD, your immune system is overactive. Something that may cause temporary airway inflammation in a healthy person may cause permanent and irreversible damage to a COPD patient’s lungs because the slightest irritant may result in prolonged inflammation.
High White Blood Cell Count
While a high white blood cell count in and of itself is not harmful, it is a sign of inflammation, chronic disease, and other symptoms. Since white blood cells are what combat infections, cancerous cells, and viruses in the body, a high WBC count is an indication that your body perceives a threat and is trying to eliminate it.

A study published in the National Center for Biotechnical Information looked at WBC counts between 1,227 COPD patients and 8,679 non-COPD adults over the age of 40. It concluded that high WBC counts were negatively associated with forced vital capacity (FVC) and forced expired volume in one second (FEV1), both of which are crucial for quality of life in COPD patients.
When an inflammatory response is triggered, phagocytes are what accelerate the amount of inflammation needed to treat the infection. They recruit alveolar macrophages that combat and control the inflammation. While alveolar macrophages are increased in patients with COPD, their ability to fight infection is impaired. This, along with a high survival rate of neutrophils leads to a high neutrophil load in the airway and a higher white blood cell count.
Reduced Number of Dendritic Cells
Dendritic cells are responsible for processing antigens and presenting it to the T cells. They are also the primary line of communication between the adaptive and innate immune system. While researchers have yet to determine exactly how dendritic cells are affected by COPD, some studies have shown that nicotine exposure can reduce the number of dendritic cells in the body while reducing their functionality, thus compromising both the innate and adaptive immune systems and their ability to work together effectively.

The Immune System and Acute Exacerbations
An acute exacerbation of COPD is a sudden worsening of respiratory symptoms and can last as short as two days or as long as a week. Acute exacerbations are more common in later stages of the disease and exhibit signs such as increased sputum (a mixture of saliva and mucus), breathlessness, coughing, wheezing, and more. Acute exacerbations are typically triggered by environmental factors such as air pollution, dirt, dust, or pollen, and infectious disease
Studies have shown that the majority of exacerbations are caused by respiratory illness like the human rhinovirus, influenza, and respiratory syncytial virus. More specifically, around half of the infective exacerbations caused by bacteria are the result of Haemophilus influenzae (NTHi) which, despite its name, is not the same thing as influenza (the flu). Due to a changing lung microbiome, impaired airway system, and unusual inflammatory response, this provides an ideal environment for it to survive in the lower respiratory area.
How To Avoid Getting Sick
Now that you know a little bit about how the immune system works and how COPD impairs your immune system, you need to know what you can do about it. No matter what stage of COPD you are in, your age, or your overall health, you should adhere to a strict routine that will keep you from getting sick and keep you breathing freely and effortlessly. While you should be doing everything you can to prevent respiratory infection, you’ll need to know how to react if you do get sick.
Quit Smoking
Smoking cessation should always be your first step in getting healthy and preventing respiratory infection. Cigarettes are what’s called an “immunosuppressive drug.” What this means is that when you smoke cigarettes, your immune system is weakened, and your body will be less prepared to fight off harmful viruses and bacteria.
 According to a study published in the Oncotarget Open Access Journal, cigarette smoke damages adaptive immune cells like regulatory T cells, B cells, and memory T/B lymphocytes while damaging innate immune cells such as natural killer cells, macrophages, and dendritic cells. What’s more, smoking increases mucus production and makes it more difficult to clear meaning harmful pathogens are more likely to build up in the lungs.
According to a study published in the Oncotarget Open Access Journal, cigarette smoke damages adaptive immune cells like regulatory T cells, B cells, and memory T/B lymphocytes while damaging innate immune cells such as natural killer cells, macrophages, and dendritic cells. What’s more, smoking increases mucus production and makes it more difficult to clear meaning harmful pathogens are more likely to build up in the lungs.
Get Plenty of Sleep
A great night’s sleep every night helps ensure your immune system is working its best. According to the National Sleep Foundation, sleep deprivation mainly affects one protein in the body: cytokines. This protein targets and prevents infection and inflammation in the body and they’re mainly produced and released while you’re sleeping.
If that’s not enough, when you slack on sleep, you’ll be more sleepy and less prepared to handle any symptoms of breathlessness or fatigue related to COPD. Getting enough sleep will give you the energy you need to follow your treatment plan to a T without making any mistakes.
Stay Hydrated
There’s no understating the importance of hydration for COPD patients. Although everyone, regardless of whether they’re healthy or sick should be getting enough water, it’s especially important for anyone with a respiratory condition. Every cell in the body needs water in order to function, including all of the immune cells that we discussed above. The human body is made of more than 50 percent water but we’re constantly losing it through sweat, urine, and breathing, so you need to replace it by consuming more.
.jpg?width=416&name=water%20(1).jpg)
Mucus is another aspect of the immune system that’s impacted by hydration. When you drink plenty of water, mucus becomes less viscous and is cleared more easily from the airways. However, if you don’t drink enough, it will become viscous and significantly increase your risk of getting sick. What’s more, if you drink water while you’re sick, it will help you to get better sooner.
Manage Stress
Stress can be a silent killer for many people’s immune system simply because it’s the last thing anyone suspects. Unfortunately, high and prolonged stress can have a number on not just the immune system, but our overall health and wellbeing. According to Simply Psychology, stress reduces the effectiveness of the immune system and lowers the number of lymphocytes by producing a hormone called corticosteroid. This hormone weakens the immune system meaning you’ll have to work harder to prevent getting sick.
Practice Good Hygiene
Maintaining great personal hygiene is an easy way to prevent infection. Be sure to wash your hands frequently, shower once a day, and if you use oxygen equipment like a home oxygen concentrator, portable oxygen concentrator, or oxygen tank, clean it at least once a day, especially the nasal cannula that actually administers the oxygen.

Follow Your Treatment Plan
Last, but certainly not least, sticking to your treatment plan will help you stay healthy. Every case of COPD is different and other factors such as your age, gender, and other conditions you may be facing may have an effect on your treatment plan. Although the immune system is sensitive, it will work its best if you maintain an optimal diet, keep up with oxygen therapy, and exercise the way your doctor recommends.
Conclusion
The immune system is an extremely complex system of cells, substances, and functions that all work together to protect your body from harm. Naturally, when a disease like COPD damages the tissues in the airways and lungs, it will have adverse side-effects on the immune system. What’s more, a weakened immune system puts COPD patients at a higher risk of contracting acute respiratory illness which results in exacerbations and causes inflammation in the lungs to progress more quickly.
Ultimately, the best way to deal with a weakened immune system is to simply follow your doctor’s instructions and don’t be afraid to ask questions. If you have any concerns, it’s best to address them sooner rather than later so that your doctor can begin to put together a solution that will prevent the exacerbation of your COPD symptoms. If you’re looking for something to do right now to boost your immune system, however, drink more water, get more sleep, and toss the cigarettes.


.png)






