
Cystic fibrosis is a rare disease caused by a genetic mutation that can be passed down from parent to child. Although there is no known cure, there are many treatments and medications for cystic fibrosis that can help reduce the effects and symptoms of the disease.
The most prominent symptom of cystic fibrosis is abnormal, thick mucus that builds up in the lungs and other organs. This causes blockages and infections that can cause a variety of serious complications, including lung disease, liver disease, and gastrointestinal (GI) problems.
Many people with cystic fibrosis fail to grow and thrive as children and experience frequent infections and organ damage throughout their lives. It is a deadly disease, and the median age of survival for people with cystic fibrosis is around 40 years old.
Cystic fibrosis is complex and affects many different parts of the body, including the lungs, pancreas, liver, and intestines, in different ways. People with cystic fibrosis have to take a variety of medications, adhere to special diets, and do daily respiratory exercises to combat serious problems like malnutrition and difficulty breathing.
Symptoms of cystic fibrosis usually show up very early in life, and most people are diagnosed by the time they turn two. The disease requires daily, life-long management to keep uncomfortable symptoms at bay and prevent serious damage to the respiratory tract, digestive system, and other organs.
Cystic fibrosis is a life-altering condition that requires intensive treatment to manage. However, recent advancements in cystic fibrosis treatment have made huge steps toward improving patents' lifespans and quality of life. With proper medication, strict daily treatment regimens, and close monitoring from doctors and specialists, people with cystic fibrosis are now able to live better and longer than ever before.
In this article we will introduce you to the signs and symptoms of cystic fibrosis and how the disease effects many different parts of the body. You'll learn about cystic fibrosis treatments, potential complications, and how the disease gets passed down through generations.
What is Cystic Fibrosis?
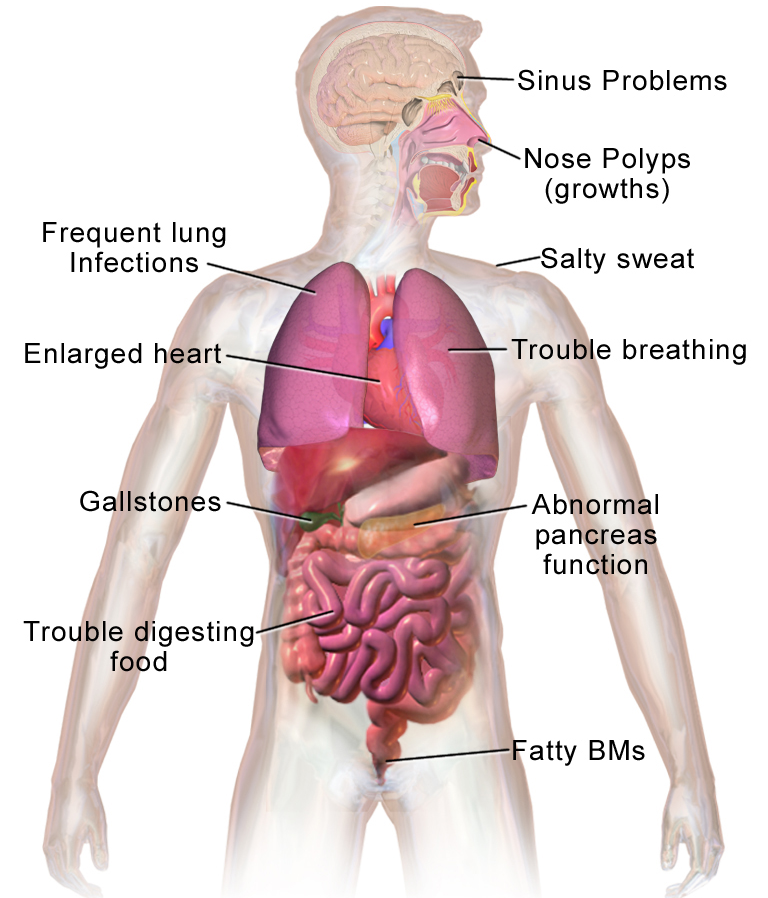
Cystic fibrosis can be difficult to understand because it comes with such a wide range of varied symptoms and complications. It doesn't just damage lungs or one type of tissue; it can affect many different parts of the body.
All people with cystic fibrosis have a mutation in a gene that controls a vital protein called the cystic fibrosis trans-membrane regulator (CFTR). This protein is an important part of membranes found all throughout the body, specifically in tissues that secrete mucus like the lungs and intestines.
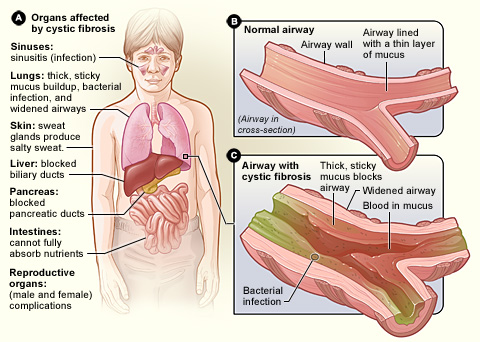
These tissues are responsible for producing thin, watery mucus to coat the insides of the lungs and other organs. This lubricates and protects the delicate inner membranes, but can be problematic if it gets too dry and thick.
A normal, functioning CFTR protein is necessary for the body to be able to secrete normal mucus as well as thin, flowing fluids that other organs, like the pancreas, produce. Unfortunately, people who have cystic fibrosis don't have enough of this protein working in their bodies.
That is because a genetic defect causes one of two things to happen:
- The body makes an abnormal version of the CFTR protein that doesn't function properly.
- The body can't make enough of the CFTR protein.
In either case, this results in mucus and other secretions that don't function properly. Instead of producing thin, flowing mucus, people with cystic fibrosis produce dry, thick mucus that sticks to insides of their lungs and other organs.
This thickened mucus can't do its job and instead clogs up organs and provides an ideal spot for bacteria to grow. It also has specific effects on the liver, gut, and pancreas that disrupt their normal function and can lead to serious disease.
How Cystic Fibrosis Affects Your Body
Cystic fibrosis symptoms vary from person to person,and there are multiple types of CFTR gene mutations that can cause the disease. Every case of cystic fibrosis is different, and some are more severe than others.
But one thing all people with cystic fibrosis share is a buildup of excess mucus and phlegm in their bodies, especially in their lungs and digestive tract. This is because the defective CFTR protein cannot properly regulate the water content of the body's secretions, leading to mucus that's extra thick and sticky, instead of thin and free-flowing.
This has a devastating effect on many parts of the body, and we'll go through them here one by one.
Lungs
When you have cystic fibrosis, the thickened mucus in your lungs dries up easily and clogs up your airways. This thick, sticky mucus is difficult to clear out and sits in place, inviting bacteria to build up in the airways and infect the lungs.
The mucus buildup blocks air from flowing through your lungs easily, causing breathlessness, coughing, and reduced lung function. One of the most important parts of cystic fibrosis treatment is clearing mucus out of the airways and keeping the lungs as healthy as possible.
People with cystic fibrosis often suffer from frequent or chronic lung infections that can cause a chronic, phlegmy cough and difficulty breathing. The constant irritation and inflammation damages the lungs over time and can eventually lead to lung disease, heart disease, and death.
Sweat

Besides mucus, the CFTR protein also regulates other substances the body makes, like sweat and digestive fluids. In people with cystic fibrosis, the defective CFTR protein causes their bodies to excrete too much salt in their sweat, which depletes salt levels in the rest of the body.
If you have cystic fibrosis, this can cause serious problems during exercise or when spending time in the heat. Sweating can quickly lower salt levels in the body to dangerous levels, leading to severe dehydration, fatigue, muscle cramps, and even heat stroke.
That's why people with cystic fibrosis have to take extra care to stay hydrated, especially during physical activity. Drinking fluids like sports drinks that contain salt and other electrolytes can help replenish your salt levels, too.
Liver

Bile is an important digestive fluid that's released into your stomach when you eat food. This bile is made by the liver and passed to the gallbladder, where it is stored until it's needed.
Cystic fibrosis affects the bile-producing cells in the liver, causing them to secrete bile that's thicker than the usual flowing fluid. This can clog up t he liver and gallbladder and cause obstructions in the ducts that carry the bile, leading to liver scarring, gallstones, and other complications.
he liver and gallbladder and cause obstructions in the ducts that carry the bile, leading to liver scarring, gallstones, and other complications.
Pancreas
The pancreas is a vital part of the gastrointestinal system because it secretes the digestive enzymes needed to break down food. Cystic fibrosis affects the cells that secrete the pancreatic enzymes, causing the secretions to become thick and clog up the pancreas.
When this happens, enzymes are unable to make it into the intestines where they are needed to digest food. As a result, it doesn't get broken down correctly and the body cannot absorb the nutrients from the food you eat.
These nutrients are necessary for the body to grow and function, and untreated cystic fibrosis leads to illness and malnutrition. That's why 90 percent of people with the disease have to take pancreatic enzyme supplements with every meal—to make up for their pancreas's inability to supply its own digestive enzymes to the digestive tract.
The pancreas is also responsible for producing insulin, the substance that controls the amount of sugar in your blood. Cystic fibrosis can cause cysts and blockages in the pancreas that cause scarring and damage to the cells that make insulin.
Cystic fibrosis gets its name from these cysts that can develop in the pancreas as a result of the disease. However, it is not a very common occurrence, and only about 15 percent of people with cystic fibrosis develop this condition.
Intestines

Cystic fibrosis affects fluids secreted in the intestines, causing constipation and sometimes intestinal blockages. This happens because there is not enough water in the stool, and it can cause a serious condition in newborn babies called meconium ileus, which requires surgery.
Furthermore, cystic fibrosis prevents the pancreas from delivering digestive enzymes to the gut, which can cause serious complications in the gastrointestinal tract. This makes people with cystic fibrosis prone to malnourishment and symptoms like cramping, bloating, and constipation caused by undigested food that the body is unable to break down.
In the most severe cases, people with cystic fibrosis can have severe intestinal obstructions that completely block the intestines. Rectal prolapse is another complication that can arise from constant straining due to constipation and unusual bowel movements.
Key Facts about Cystic Fibrosis
Cystic fibrosis is a relatively rare disease, affecting about 30,000 people in the United states and up to 100,000 people worldwide. Although there is no way to cure the disease, there are many treatments available that focus on improving the symptoms, lifespan, and quality of life for people living with cystic fibrosis.

There are at least 1,700 different genetic mutations that can cause cystic fibrosis, and perhaps even more that haven't been studied. However, the vast majority of cystic fibrosis cases are caused by a single type of mutation, known as the F508 mutation. The rest are caused by one of the other hundreds of possible mutations.
The disease is serious, progressive, and tragically shortens the lifespan of people who suffer from it. However, with modern therapies people with cystic fibrosis are able to live much longer, better lives than ever before in history.
Until the late 1900's, most people born with cystic fibrosis didn't survive past elementary school. However, with proper treatment and medication the current median lifespan for people with cystic fibrosis is about 40 years old, and some live much longer.
Most cases of the disease are caught very early, often in newborn babies. In fact, hospitals have been required to do genetic screening for all newborns since 2010 to look for signs of cystic fibrosis. It's been very successful, and now nearly 65 percent of cystic fibrosis cases are found through newborn screening.
Cystic Fibrosis Symptoms
Since the disease is genetic, people with cystic fibrosis are born with it and usually start showing symptoms very early on in life. It is important to catch and begin treating the disease as early as possible to prevent serious complications and death.
The most prevalent and noticeable symptoms are coughing, phlegm, and shortness of breath. Many people with cystic fibrosis also fail to thrive and grow as children, and have difficulty putting on weight.
Cystic fibrosis is very taxing on the body and causes people with the disease to burn more energy and have large appetites. However, because their intestines aren't able to absorb nutrients efficiently, people with the disease are prone to getting malnourished and have difficulty gaining weight despite eating plenty of food.
Early-life Symptoms of Cystic Fibrosis:
- Salty skin and sweat
- Huge appetite (or reduced appetite, in some cases)
- Weight loss or difficulty putting on weight (failure to thrive)
- Low energy and fatigue
- Difficulty breathing
- Chronic coughing or wheezing
- Unusual bowel movements, such as constipation, chronic diarrhea, or large, greasy or foul-smelling stools.
Later-life Symptoms of Cystic Fibrosis:
- Difficulty breathing, especially with exercise
- Frequent lung infections
- Chronic cough with phlegm or blood
- Rectal prolapse from excessive straining
- Growths (polyps) in the nose and sinuses
- Clubbing (rounding and swelling) of the fingers
- Infertility
Causes of Cystic Fibrosis
Cystic fibrosis is an autosomal recessive genetic disease. That means that the only way you can get cystic fibrosis is if you are born with two defective copies of the CFTR gene; one inherited from each parent.

As we've explained, cystic fibrosis is a heritable disease that you have from birth, caused by mutated CFTR genes. There are around 1,700 different DNA mutations that can cause cystic fibrosis, but all of them lead to a defective CFTR protein that causes the body to secrete thickened mucus in the organs and airways.
Every person has two different versions of every gene, including the CFTR gene. Cystic fibrosis can be passed on to a child when two parents, who each have at least one defective CFTR gene, have a baby.
If the baby inherits one mutated gene and one normal gene from its parents, it would be a carrier of the disease, but not have any of the symptoms. Carriers can pass on the disease to to their own children, but only if they have a child with someone who is also a carrier.
When two parents who are carriers for cystic fibrosis have a baby, there is a 50% chance that the baby will receive one defective copy of the gene and be a carrier itself. There's a 25% chance the baby will inherit two defective copies of the gene and get cystic fibrosis.
Newborn babies are routinely given a genetic screening to test for the most common cystic fibrosis mutations. This test also catches many people who are carriers. However, since there are nearly two thousand different genetic mutations that can cause cystic fibrosis and possibly more undiscovered, genetic screening misses some babies who carry one defective copy of the gene.

Many doctors recommend that people who are carriers of cystic fibrosis and their partners get genetic screening and counseling if they plan to have a child.
Complications with Cystic Fibrosis
Infertility
The thickened mucus and other secretions caused by cystic fibrosis can lead to infertility in both males and females. That's because the fluids in the reproductive system are thickened and prone to causing blockages.
In males, thick secretions block the ability of sperm to pass through the testes, leaving men with cystic fibrosis unable to have children. Up to ninety percent of males with the disease are infertile.
In the female reproductive system, thickened mucus in the cervix can block sperm from passing into the uterus and fertilizing the egg, causing infertility. However, infertility is much less common in females than in males.
Liver Disease
In rare cases, thickened secretions caused by cystic fibrosis can cause bile to get stuck in the bile ducts in the liver. This causes an obstruction that leads to inflammation and scarring (cirrhosis).

Only about 5-10 percent of people with cystic fibrosis develop liver disease, and it is most often diagnosed before the age of 15. Still, doctors often recommend yearly liver screenings for people with cystic fibrosis to check for scarring and inflammation.
If you have cystic fibrosis, you can improve your chances of keeping a healthy liver by taking your medication properly, practicing good nutritional habits, and avoiding excessive alcohol use.
Pulmonary Hypertension and Heart Disease
Long-term respiratory issues can cause increased pressure in the lungs that compresses the surrounding blood vessels. Over time, this can cause pulmonary hypertension, a condition in which the pulmonary (lung) arteries get constricted, raising blood pressure in the lungs.

This puts back-pressure on the heart and forces it to work harder whenever it pumps blood through the vessels in the lungs. This extra strain causes the right ventricle (bottom-right chamber of the heart) to become enlarged over time.
This greatly weakens the heart and can cause edema (swollen legs and abdomen) and shortness of breath. Eventually, pulmonary hypertension and the associated enlarging of the right side of the heart can lead to right-sided heart failure (cor pulmonale) and death.
Gallbladder Disease
The gallbladder is responsible for collecting and storing the bile secreted by the liver. In people with cystic fibrosis, the bile can become so thick that it blocks the duct that leads out of the gallbladder to the intestine.
In most cases, this doesn't cause any discomfort or symptoms, but it sometimes causes gallstones to form. This occurs in about 10 percent of patients with cystic fibrosis and is usually treated with surgery to remove the gallbladder.
Pancreatitis
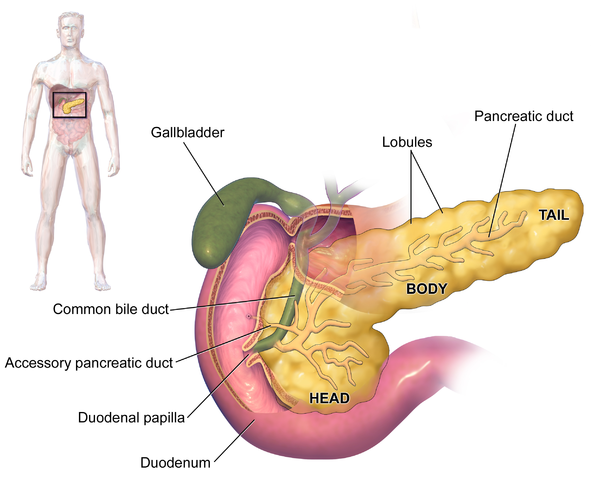
Both the gallbladder and the pancreas share a single duct that carries bile and pancreatic enzymes to the intestines. If cystic fibrosis causes gallstones to develop in the gallbladder, the stones can move up into the shared duct and block both bile and pancreatic secretions from getting through.
This can cause painful swelling and severe irritation in the pancreas, a serious condition known as pancreatitis. This can be treated with surgery to remove the gallstones or treatment in a hospital to reduce pain and discomfort until the inflammation subsides.
Bacterial Overgrowth
People with cystic fibrosis tend to develop frequent infections, especially lung infections, that require frequent courses of antibiotics. Over time, having to take antibiotics so often can kill off important, needed bacteria in the intestines.
This causes a bacteria imbalance that allows harmful bacteria to multiply. This can cause a number of uncomfortable symptoms, including nausea, gas, bloating, and diarrhea.
Bacterial overgrowth is often treated with a different kind of antibiotic that restores a healthy balance of bacteria in the gut. It selectively kills off harmful bacteria so that beneficial bacteria can thrive and flourish once more.
Diabetes and Hyperglycemia
Besides producing digestive enzymes, the pancreas has another very important purpose: secreting insulin into the bloodstream. Insulin is responsible for moving sugar out of the bloodstream and into the body's cells so it can be used as energy, and healthy insulin production is very important for overall health.
In rare cases, cystic fibrosis can cause cysts and scarring in the pancreas that destroys the cells that make insulin. Since the pancreas is the only organ that can make insulin, pancreatic scarring can severely reduce the amount of insulin in the blood.
This causes high blood sugar (hyperglycemia), which causes symptoms like dry mouth, fatigue, and frequent urination. Over time, insulin levels continue to decrease and blood sugar rises, eventually leading to diabetes.
Unlike type 2 diabetes, cystic fibrosis-related diabetes is not caused by diet or lifestyle habits, and is difficult to prevent. Fortunately, only about 15 percent of people with cystic fibrosis develop diabetes.
Gastric Paresis
Gastric Paresis occurs when food takes too long to empty out of the stomach, causing nausea, bloating, and discomfort after you eat. If you have pancreas scarring and high blood sugar, it can make the problem even worse.
Doctors often recommend that people with cystic fibrosis eat smaller, more frequent meals throughout the day to alleviate symptoms. This makes sure that you don't fill up your stomach too much, and allows it to empty more quickly and efficiently.
Delayed Puberty

Because of the digestive issues associated with cystic fibrosis, many children with the disease grow up with low body weights and nutrient deficiencies. In females, low weight and malnutrition can delay the onset of puberty.
Bronchiectasis
Bronchiectasis is a lung condition where the airways become enlarged and filled with mucus. This occurs often in people with cystic fibrosis as a result of chronic respiratory infections that inflame the airways and fill them with mucus, stretching them and causing permanent enlargement.

This makes the airways even more prone to infection in a self-perpetuating cycle that leads to more mucus, more enlargement, and more infections. This causes progressive damage to the lungs and airways over time, making it more and more difficult to breathe.
Antibiotics, expectorants, and bronchodilators are often prescribed to help treat bronchiectasis and make it easier to clear mucus from the airways. Practicing airway clearance techniques like chest percussion or postural drainage can help reduce symptoms and damage to the airways. Many patients with advanced bronciectasis require supplemental oxygen therapy as their lung function declines.
Pneumothorax

Pneumothorax is a medical term for the partial collapse of a lung. Anywhere from 5-20 percent of people with cystic fibrosis will develop a collapsed lung throughout their lifetime.
Pneumothorax is a life-threatening condition and happens when air leaks out of the lungs and fills the space around them, putting pressure on the lungs, heart, and blood vessels. This leaves less room for the lungs to expand, causing shortness of breath and pain when inhaling.
Risk Factors for Cystic Fibrosis
Since cystic fibrosis is caused by a heritable genetic mutation, you can only get cystic fibrosis if you inherit defective CFTR genes from both of your parents. Cystic fibrosis tends to occur most often in non-hispanic white people and is less common in people who belong to other racial and ethnic groups.
If you only inherit one defective gene, then you are a carrier. While carriers don't actually show any signs of cystic fibrosis themselves, they risk passing their defective gene on to their children.
Doctors recommend genetic screening to couples who plan to have children if either of them is a carrier for cystic fibrosis.
Treatments for Cystic Fibrosis

Cystic fibrosis is a complex disease that can be unpredictable and affect people in different ways. What kind of treatment your doctor recommends depends on how the disease is affecting your body and how severe your symptoms are.
Although cystic fibrosis has no known cure, there are many different ways to manage the symptoms. New drugs and medical treatments have made huge improvements in the quality of life and average lifespan of people with the disease.
Most cystic fibrosis treatment plans include medication, airway clearance techniques, and special dietary habits. Since frequent infection is a common complication, preventing and managing illnesses is another important part of managing the disease.
If you have cystic fibrosis, you will likely have to follow a daily regimen that includes enzyme supplements, inhaled medications, and airway clearance exercises. Since cystic fibrosis tends to have the most serious effect on the lungs and digestive system, keeping the lungs and gut healthy is one of the main focuses of treatment.
It is also important to maintain a healthy, active lifestyle over the long-term in order to slow down physical decline. Getting regular exercise and sticking to the diet your doctor recommends will help you maintain your overall wellness and quality of life.
Healthy Habits to Treat Cystic Fibrosis
Eat a Healthy Diet

People with cystic fibrosis have very sensitive digestive systems. Complications like constipation and intestinal blockages are common, as are stomach issues and GERD.
Because cystic fibrosis can cause your stomach to empty slowly, causing stomach distress and pain, doctors recommend that you eat several smaller meals throughout the day instead of a few large ones. This makes sure you don't overload your stomach or digestive tract with too much food at once.
Because the disease makes it difficult to absorb enough nutrients from food, people with cystic fibrosis often work with a dietician to develop a tailored diet and supplement plan. Many people with cystic fibrosis take vitamin supplements and eat a special high-calorie, high-fat diet.
When you have cystic fibrosis, it's also very important to remember to take your enzyme supplements with every single meal. Forgetting or skipping your prescribed enzyme supplements or other medications can lead to malnutrition, pain, constipation, and other serious gastrointestinal complications.
Get Vaccinated
If you have cystic fibrosis, you are more vulnerable to many kinds of illness and infections. Disease prevention is a very important part of treating cystic fibrosis, which is why you should always keep up with scheduled vaccinations and get the pneumococcal vaccine to prevent pneumonia.
Because their livers are already prone to disease, it is especially important for people with cystic fibrosis to get their hepatitis A and hepatitis B vaccines. These vaccines protect the liver from dangerous viruses that cause severe liver damage and scarring.
Avoid Alcohol

Alcohol can be toxic to the liver and pancreas. People with cystic fibrosis are advised to avoid drinking because it can cause serious damage to these organs, which are already vulnerable to disease.
Excessive alcohol use can increase your chance for liver scarring and cause severe, irreversible damage to the pancreas. In some cases this can even lead to insulin resistance and diabetes.
Get Plenty of Exercise
Some people with cystic fibrosis find exercise difficult because mucus blocks their airways, making it difficult to breathe. However, sticking to a regular physical activity regimen is an important part of keeping the heart and lungs healthy and preventing further respiratory decline.
Exercising forces you to breathe heavily and can help loosen mucus in your chest and airways, making it easier to breathe in the long run. However, it's important to regularly replenish your body's water and salt as you exercise. That's because cystic fibrosis causes your body to secrete extra salt in your sweat, leaving you prone to dehydration and salt imbalances.
Airway Clearance Techniques to Treat Cystic Fibrosis
![]()
One of the most important parts of the daily cystic fibrosis treatment regimen is clearing mucus out of the airways. This makes it easier to breathe, easier to exercise, and prevents inflammation and infection in the lungs.
In order to clear mucus out of the airways, you have to use air flow to forcefully lift and carry it out of the lungs and small airways. You can do this by coughing and huffing, which lifts and carries the mucus out of the most narrow airways into the larger airways, where it accumulates until you cough it up out of the larger airways and out of your mouth.
All airway clearance methods involve some form of coughing or huffing. Many techniques also include some form of tapping, clapping, or vibration on the chest, which helps dislodge mucus from the airways and makes it easier to cough out.
Airway clearance techniques usually work best in combination with other medications and therapies which relax and open up the airways. Your doctor will likely recommend using a bronchodilator or nebulizer before performing airway clearance techniques to make them more productive.
Basic Airway Clearance Techniques:
- Coughing: Coughing pushes a large amount of air out of your air at high speed, which helps push mucus out of the airways. It happens reflexively whenever the lungs are irritated or when mucus builds up in the larger airways, or you can induce coughing purposefully to force phlegm out of your lungs.
- Huffing: Huffing is less forceful and violent than coughing, and can be less uncomfortable and tiring. You start by taking in a deep breath in and holding it for a moment or two before expelling the air quickly. This helps force mucus out of your lungs and airways so you can cough it up.
Advanced airway clearance techniques combine coughing and huffing with other methods to more effectively expel mucus.
Postural Drainage
Postural drainage is a simple technique in which you position your body in different ways to encourage mucus to drain out of your lungs to your mouth. There are nearly a dozen postural drainage poses and each helps to drain mucus from a different section of the lungs.
Most positions require you to lie on your side, back. To allow mucus to drain, you hold each position for a short period of time, usually 3-5 minutes. You can then sit up and huff or cough to expel the mucus.
To learn all ten postural drainage positions, check out this fact sheet from the Cystic Fibrosis Foundation.
Lung Percussion
Back and chest percussion is a type of chest physiotherapy commonly used to loosen up mucus trapped in the lungs and airways. To perform this technique, you tap firmly in specific spots on your chest and back to help dislodge mucus from the walls of your airways. You might want to enlist a friend, family member, or caretaker to help.
To do this exercise, you lie flat on your stomach or back (depending on whether you are doing the back or chest) and take in a deep breath. Then you tap firmly and repeatedly on specific spots on the upper-right and upper-left side of your chest and/or back.
The proper percussion technique is to cup your hand slightly and clap it palm-side down using the motion from your wrist. The tap should be firm and rhythmic, but not painful, and make a hollow “clapping” sound.
You can also perform a vibration technique in a similar way. Instead of using percussion, you press your flat palm (or both palms) on the same areas of the upper chest and back and shake them in a vibrating motion.
After each percussion or vibration session, you should sit up and try to huff and cough up any loosened phlegm. You can ask your doctor to show you the best spots to tap on when you do chest and back percussion exercises, and you can learn more from the Cystic Fibrosis Foundation's Website.
High-Frequency Chest Wall Oscillation
This technique requires a special vibrating vest that many people with cystic fibrosis use to help them loosen mucus in their chest. The medical vest is inflatable and works by inflating and deflating rapidly, creating a vibrating sensation that dislodges mucus from the lungs and lower airways.
To use the vest, you wear it for about five minutes at a time with a few minutes in-between sessions. When you turn the vest off, spend a few minutes coughing and huffing until you're able to expel some of the phlegm.
Positive Expiratory Pressure Therapy

With this technique, you use a medical device called a positive expiratory pressure (PEP) machine. This device uses a breathing mask to deliver pressurized air into your airways, holding them open so mucus can move through them more easily.
To do positive expiratory pressure therapy, you take a deep breath through the PEP device and hold it for a few moments. Then you exhale slowly through the device for four or five seconds.
Repeat this process at least fifteen times to loosen up the mucus in your airways. After that, cough or huff to expel the phlegm, and then repeat the process again as many times as your doctor recommends.
Lung Flutes
There are special breathing devices, often called lung flutes, that vibrate when you blow air out through them. They are hand-held devices and they use oscillating positive expiratory pressure to help you cough up mucus.
The vibrations created when you exhale through a lung flute cause the small airways in the lungs to vibrate too. This helps dislodge thick mucus from the walls of your airways so you can cough it up and clear it out.
To use a lung flute, you take a deep breath in and then exhale forcefully through the mouthpiece. Like playing an instrument, it can take some time and practice to exhale in just the right way so it vibrates correctly.
After exhaling several times through the flute, you cough or huff to expel the loosened phlegm from your airways. Repeat this cycle several times to more effectively clear mucus from your lungs.
Gastrointestinal Treatments for Cystic Fibrosis

Since the buildup of thick mucus prevents digestive enzymes from entering patients' digestive tracts, people with cystic fibrosis need help digesting food properly. Fortunately, vitamin supplements and enzyme supplements can help people with cystic fibrosis better break down and absorb the nutrients they need.
Pancreatic Enzyme Supplements
The vast majority of people with the cystic fibrosis—87 percent—have to take pancreatic enzyme supplements to aid their digestion. These enzymes break down the ingredients in the food you eat in place of your own pancreatic enzymes.
Pills containing pancreatic digestive enzymes (including Pancrelipase and Pancreatin) dissolve in the small intestine, breaking down fats, carbohydrates, and proteins. This allows the digestive tract to absorb the nutrients and use them for all the body's processes.
If you have cystic fibrosis, you will need to take the right amount of pancreatic enzymes before every single meal to ensure that you can digest the food correctly. Your doctor will tell you which enzymes, and how much, you should take.
Multivitamins
Because the intestines struggle to absorb enough nutrients from the food they eat, people with cystic fibrosis often have to supplement their diets with extra vitamins. In fact, there's a special mutivitamin combination formulated specifically for people with cystic fibrosis often called an ADEK.
The ADEK vitamin formulation contains four essential vitamins that people with cystic fibrosis tend to be deficient in: vitamin A, vitamin D, vitamin E, and vitamin K1. These vitamins help support a number of vital functions, including bone development, brain development, and other biological systems.
If you have cystic fibrosis, your doctor will give you a special supplement regimen tailored to your age, weight, and individual problems.
Inhaled Medications for Cystic Fibrosis

There are several types of medications commonly used to treat cystic fibrosis that are inhaled through a nebulizer or inhaler. A nebulizer is a machine that takes a liquid medication and turns it into a mist that you can breathe in to your lungs.
Many cystic fibrosis patients have reusable nebulizers at home that they use to inhale medications and saline solutions daily. It's extremely important to properly clean and care for your reusable nebulizer to prevent infections and the spread of bacteria.
Bronchodilators
Bronchodilators are a type of inhaled medication that helps relax and dilate (widen) airways in the respiratory tract. This makes it easier to breathe and easier to move thick mucus out of the tiny, narrow airways and into the larger ones where it can be coughed up and out of the lungs.
Because they open up the airways and make it easier to move more air through the lungs, doctors often recommend using a bronchodilator before doing other treatments like airway clearance techniques. It can also help the lungs more efficiently and effectively absorb inhaled medications like mucolytics and hypertonic saline solutions.
Drugs that act as bronchodilators include albuterol and levalbuterol hydrochloride. They are most often used with an inhaler, but they are also sometimes inhaled through a nebulizer or a dry powder.
Mucolytics
Mucolytics, or mucus thinners, are an important part of any cystic fibrosis treatment plan. These drugs help treat the primary symptom of cystic fibrosis: thick, sticky mucus that builds up in the lower airways.
Mucolytics help to thin the mucus by breaking down materials, like proteins and DNA, that accumulate in the mucus and cause it to become even thicker. This makes it easier to cough up and clear mucus from the lungs and lower airways, which you can do by practicing airway clearance techniques.
Drugs like Dornase Alfa are mucolytics, but non-drug treatments like hypertonic saline can thin mucus, too. Mucolytics are inhaled through a nebulizer and only stay active in the body for a short period of time. Because of this, it's important to perform airway clearance exercises immediately after taking mucolytics.
Both Dornase Alfa and hypertonic saline are commonly used together, and doctors often recommend using a bronchodilator in combination with mucolytics to make them even more effective.
Salt Water Solution (Hypertonic Saline)
Sterile salt water solutions can be misted through a nebulizer and inhaled in order to thin mucus. Studies show patients with cystic fibrosis can benefit from fewer lung infections and respiratory symptoms when they inhale hypertonic saline twice every day.
When you inhale salt water, it coats your lungs and upper airways with sodium. This encourages more water to move into the airways via osmosis, which thins the mucus there and makes it easier to get out using airway clearance techniques.
Other Medications for Cystic Fibrosis
Doctors prescribe a variety of medications to control the varied symptoms, infections, and organ problems caused by the disease. There are even a few drugs developed specifically to treat the underlying cause of cystic fibrosis, although they are only effective at treating certain forms of the disease.
Medicines to Reduce Inflammation

There are a several different medications that are effective at treating inflammation in people with cystic fibrosis. People with the disease often need them because they experience chronic lung infections and inflammation day after day, which can cause irreparable damage to the lungs.
People with cystic fibrosis usually have an excessive, overly intense inflammation response that reacts strongly to even mild irritation. Anti-inflammatory drugs help protect the lungs by calming and dampening the body's inflammation reaction, which improves lung function and protects the lungs from disease.
Common, over-the-counter NSAIDs (Non-steroidal anti-inflammatory drugs) like ibuprofen, or prescription-strength versions, are often used to treat mild inflammation in people with cystic fibrosis. In some cases doctors prescribe corticosteroids (such as prednisone and fluticasone), but they can have serious side effects and should only be used for short periods of time.
Patients with cystic fibrosis often take anti-inflammatory drugs to help them recover from short-term infections and exacerbations. They are also sometimes prescribed for everyday use and can help reduce swollen airways and improve lung function.
CFTR Modulator Therapies
There are two different CFTR drug therapies that were developed specifically to treat certain cases of cystic fibrosis. These medications can be very effective at treating the underlying cause of the disease, but it only works for people whose disease is caused by one of a few specific CFTR gene mutations. Patients with different mutations have to rely on other treatments.
The two FDA-approved medications ivacaftor and lumacaftor work by acting on the defective CFTR protein to make it more functional. Ivacaftor—which works for at least 10 different cystic fibrosis mutations—helps increase the activity of the CFTR protein.
Lumacaftor works for the most common cystic fibrosis mutation, the F508 mutation that is responsible for about 70 percent of cystic fibrosis cases. This medication helps move defective CFTR proteins into the right place in the membrane of the cell so they can do their job correctly.
The Cystic Fibrosis Foundation actively funds continuing research and development of drugs that treat the underlying causes of the cystic fibrosis, and hopes to develop treatments to help people with many different CFTR mutations. If you have cystic fibrosis, you can get free genetic testing from the Cystic Fibrosis Foundation to figure out exactly which mutation you have and if there is a CFTR treatment that will work for you.
Other Medical Treatments for Cystic Fibrosis
Antibiotics

Thickened mucus that sits in the airways invites bacteria to thrive and multiply. That's why cystic fibrosis causes sufferers to get lung and respiratory infections often.
When this happens your doctor will give you antibiotics to kill the bacteria and get rid of the infection. In some cases, doctors will prescribe inhaled antibiotics as part of a daily treatment routine to stave off infections and complications.
There are a wide variety of antibiotics available to use depending on the type and severity of infection. In extreme cases, such as when you experience an exacerbation, patients have to have antibiotics injected directly into their bloodstream through an IV.
It is very important to take antibiotics exactly as directed by your doctor, and to finish every course of antibiotics as instructed. Antibiotic resistance is a major risk for people with cystic fibrosis, and misusing them greatly increases the chance for antibiotic-resistant infections.
Supplemental Oxygen Therapy
Lung infections and blocked airways caused by cystic fibrosis can severely hurt your lung function. The lack of air flow through the lungs leads to low blood oxygen levels, and over time can cause serious heart and lung complications.
Damage and scarring in the lungs makes them less able to absorb oxygen and can cause dangerous conditions like pulmonary hypertension and heart disease. That's why it's so important to clear mucus from the airways, prevent lung infections, and make sure the lungs are getting enough oxygen to the rest of the body (hypoxia).
When the lungs become damaged and scarred, supplemental oxygen is often used to prevent hypoxia and keep the lungs healthy. Some people only need to take supplemental oxygen at night or during physical activity, but some patients with severe lung decline need supplemental oxygen all throughout the day.
There are a variety of medical devices you can use to get supplemental oxygen, including portable battery-powered concentrators and oxygen tanks. Your doctor will help you decide how much supplemental oxygen you need and when you should us it.
Lung Transplant
If lung disease becomes very severe, it can lead to heart problems, respiratory failure, and death. In such cases, lung or heart-lung transplant surgery can sometimes be an option for people with cystic fibrosis-related end-stage lung disease.
This is a very serious operation that takes a lot of time and requires working with a variety of medical specialists. In order to be eligible for a transplant, you have to be in good enough health to survive and thrive after the surgery.
If approved for a lung transplant, you'll be placed on a list to wait for a compatible organ donor. After the surgery, people who receive new organs have to take medication that suppresses their immune system for the rest of their lives to prevent their body from rejecting the organ.
Conclusion
Cystic fibrosis is a difficult disease to live with and requires life-long treatment to keep in check. Although there is no way to completely cure cystic fibrosis, ongoing research has led to the development of cystic fibrosis-specific medications that can treat the underlying cause of disease in many people.
People with cystic fibrosis have to work closely with many types of medical specialists and follow intensive daily treatment plans in order to keep the disease at bay. Daily medication, inhalers, airway clearance techniques, and dietary supplements are all important parts of an effective treatment plan.
Because of new drugs and therapies, people with cystic fibrosis are able to live much better, longer lives than in the past. As recently as the 1950's, children born with cystic fibrosis rarely lived long enough to grow up or go to school.
Now, the life expectancy for people with cystic fibrosis has increased significantly, with a median age of survival of about 40 years old. This has allowed people with the disease to grow up, have families, and live life to the fullest.

Organizations like the Cystic Fibrosis Foundation continue to fund research into medications and therapies for the disease. There is hope that, in the future, there will be more specialized treatments to help even more people who suffer from cystic fibrosis live better, healthier, and longer lives.


.png)


