Although COPD is known primarily as a lung disease, some of its most serious complications have to do with the heart. People with COPD tend to struggle with a variety of cardiovascular symptoms and complications, including cardiovascular disease, heart attacks, and heart failure.
Heart disease is the number one cause of death in the US, and is also one of the most common killers of people with COPD. However, the risk of heart attacks and heart failure for COPD patients is significantly higher than it is in the general population, even in patients who don't have other heart problems.
Because of this, keeping your heart and cardiovascular system healthy is a critical part of COPD treatment. Keeping your heart strong can actually reduce COPD symptoms as well as prevent serious, life-threatening complications like heart attacks.
In this article, we're going to explain how COPD affects the heart and why the disease raises your risk of having a heart attack. We'll also show you what you can do to prevent heart attacks and keep your heart healthy with COPD.
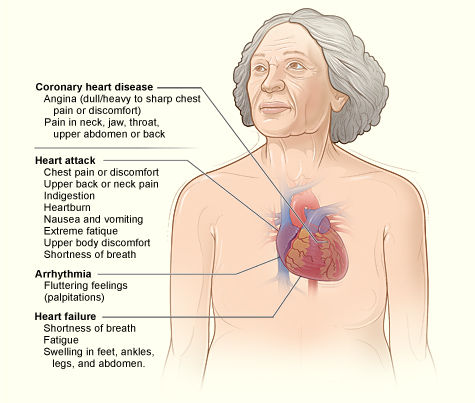
Symptoms of a Heart Attack

A heart attack happens when your blood vessels become so narrowed that it cuts off blood flow to the heart. This can happen as a result of a blood clot, high blood pressure, and clogged arteries, which are often the result of heart disease.
Doctors and researchers don't fully understand exactly why many heart attacks happen, or through what exact mechanism COPD causes sudden heart attacks. However, they do understand the major risk factors, which include smoking, high blood pressure, high cholesterol, obesity, stress, and diabetes.
The earlier you get treatment for a heart attack, the more likely you are to survive and avoid serious, permanent damage to your heart. Because of this, it's very important to know the symptoms of a heart attack and how to recognize them, especially if you have COPD.
However, heart attacks don't feel the same for every person and the symptoms can vary widely from case to case. Some people experience severe chest pain or fainting, while some feel little pain or hardly any symptoms at all.
Some heart attacks happen suddenly, with little warning and few symptoms, but some develop slowly over the course of hours, days, or weeks. The most reliable symptom to look for is chest pain, especially chest pain that gets worse with activity and gets better with rest.
Here are some of the most common symptoms of a heart attack:
- Chest pain that may feel like any of the following: pressure, tightness, squeezing, or aching.
- Chest pain that spreads to your arm, neck, jaw, or back.
- Heartburn
- Abdominal pain
- Nausea
- Shortness of breath
- Sudden dizziness or lightheadedness
- Fainting
- Cold sweating
- Fatigue
If you notice the symptoms of a heart attack, you should seek medical attention immediately. Have someone drive you to an emergency room or call 911 right away.
Don't ever ignore the warning signs of a heart attack; it's better to get checked by a doctor—even if it might be nothing—than to wait too long and risk suffering severe heart damage or death. Getting to an emergency room at the first sign of a heart attack will give you the greatest chance of recovery.
How COPD Raises Heart Attack Risk
People with COPD tend to get heart disease earlier and are more likely to suffer heart failure and die from cardiovascular problems. Even COPD patients who don't have cardiovascular disease or other heart complications have a much higher risk of sudden cardiac death.
According to one study, living with COPD more than doubles your risk of sudden cardiac death, and the risk gets even higher for patients who have worse COPD symptoms and complications. Because of this, researchers are beginning to consider COPD an independent risk factor for heart disease and heart attacks, akin to high blood pressure and diabetes.
To understand why COPD causes heart attacks, you have to understand how the disease affects the cardiovascular system, including the heart, blood vessels, and pulmonary arteries (blood vessels in the lungs). These critical organs and tissues sustain damage over time as your body is affected by COPD, eventually leading to complications like cardiovascular disease, heart attacks, and heart failure.
The Heart-Lung Connection

Heart disease is a leading cause of death for all people in the US, not just people with COPD. However, COPD patients' heart problems are directly tied to their disease, which damages the heart in a specific way.
To understand how COPD causes heart problems, you have to first understand how the function of heart and lungs are intimately and inextricably linked. The heart and lungs work together in synchrony to supply your body with oxygen and remove waste, like carbon dioxide, from you body's tissues. If either organ is damaged, the other organ, and the whole cardiovascular-respiratory system, suffers too.
In fact, it's hard to overstate how much the heart and lungs rely on one another to function. The heart takes in oxygen-poor blood from the body and pumps it straight into the lungs to become oxygenated again. As the blood travels through the pulmonary arterties (blood vessels in the lungs), it absorbs oxygen and goes right back into the heart, where it pumps the now-oxygen-rich blood back throughout the body.
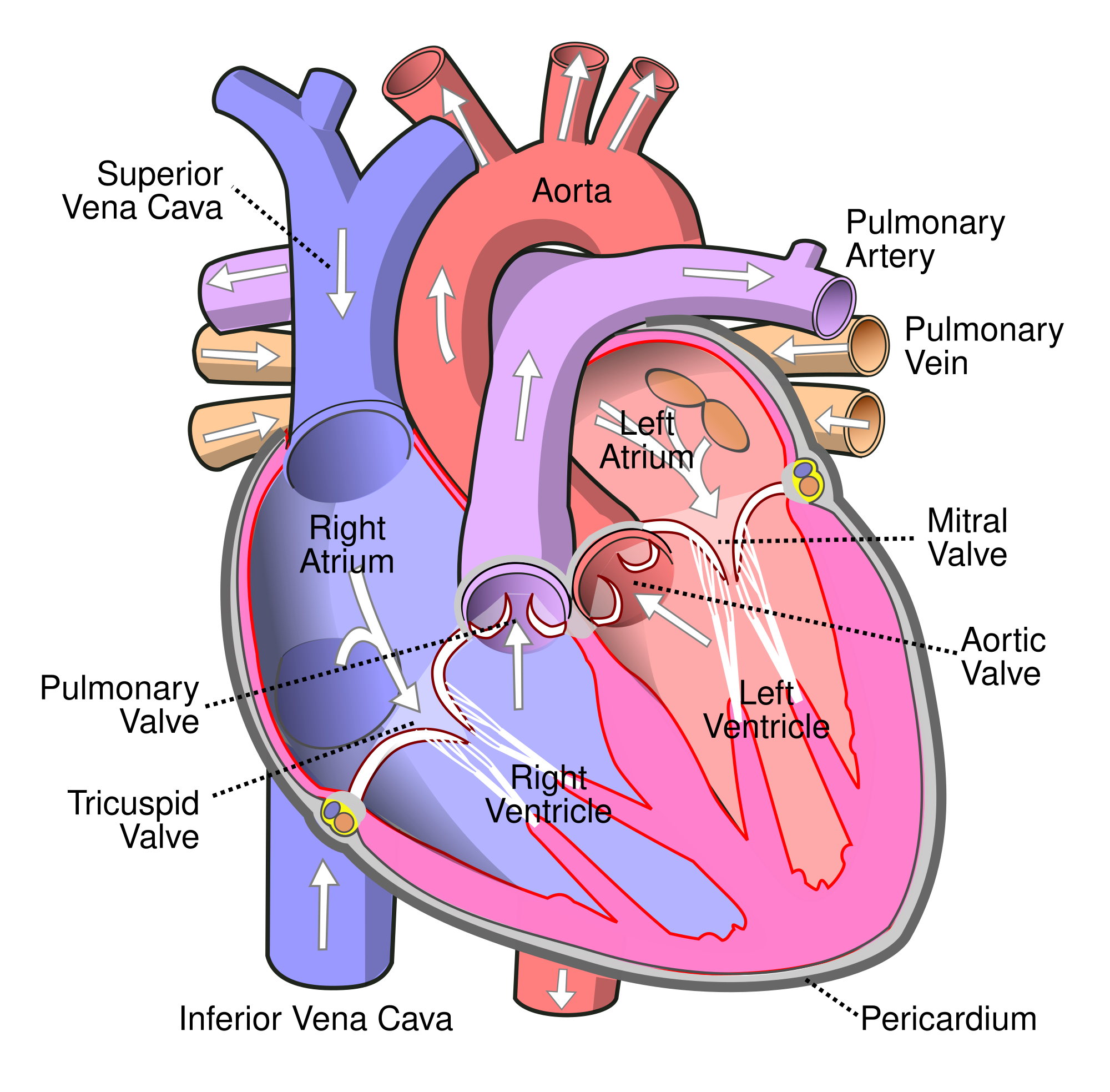
But in order to absorb oxygen, your blood must pass through the alveoli, the tiny air sacs in your lungs that allow oxygen to pass from the air into your blood. However, people with COPD have many damaged, non-functioning alveoli, so they aren't able to absorb as much oxygen as healthy lungs can.
COPD also causes inflammation in the lungs, which further damages alveoli and reduces the lung's ability to absorb oxygen even more. Eventually, lung function declines so much that the blood that passes through the pulmonary arteries doesn't get fully oxygenated, resulting in low blood oxygen saturation levels (a condition known as hypoxemia).
How COPD Strains the Cardio-Respiratory System

The main problem that people with COPD have is that their lung function is severely limited. Damaged air sacs and airway obstruction makes it difficult for the lungs to absorb enough oxygen causing serious respiratory symptoms and hypoxemia.
Hypoxemia is very bad for your body, and the heart tries to compensate for the low blood oxygen levels by pumping faster and harder. This increases the blood pressure in your lungs, which in turn creates extra back-pressure on the heart as it tries to squeeze extra blood into the pulmonary arteries.
Over time, the back-pressure that it puts on the heart causes the heart to swell and enlarge. This makes the heart walls weaker and makes it even more difficult for your heart to pump blood. These lung problems get worse and worse over time, all the while putting more and more strain and pressure on the heart.
This cycle continues, and, over time, makes your heart larger, weaker, and less effective at pumping blood through your body. As your COPD gets more severe, so does the strain on your heart, which significantly increases your risk for heart attacks and heart failure.
Pulmonary hypertension can also happen when blood vessels in the lung become narrowed and stiffened, as a result of airway obstruction caused by COPD. This also causes high blood pressure in the lungs and creates back-pressure in the heart every time it tries to pump blood into the pulmonary arteries.
Over time, this enlarges and weakens the heart, making it more and more difficult to pump blood through the lungs. If the heart becomes too weak and enlarged, it can fail, causing right-sided heart failure.
COPD and Cardiovascular Disease
Recent studies have shown that cardiovascular disease is much more common in people with COPD than was once believed. Researchers believe that this may be directly related to inflammation rather than breathing problems related to COPD.
COPD causes chronic inflammation throughout the body, not just in your lungs. One of the places this inflammation does the most damage is in the arteries, where it leads to plaque build-up and cardiovascular disease.

Beacause of this, inflammation is another major factor contributing to the increased incidence of cardiovascular disease in COPD patients. Cardiovascular disease includes high blood pressure, stroke, heart disease, coronary artery disease, and artherosclerosis.
How to Reduce Your Risk of Heart Attacks and Heart Failure if You Have COPD
Now that you understand how COPD causes heart attacks and cardiovascular complications, you need to know how to protect your heart from the strain caused by the disease. Luckily, there are plenty of things you can do in your everyday life to strengthen your heart and improve your cardiovascular health.
In this next section, we'll show you how to make heart-healthy choices and reduce your risk of having a heart attack if you have COPD. We'll give you a variety of tips and techniques for reducing your risk of COPD-related heart complications including how to monitor your blood oxygen, eat a heart healthy diet, and how to exercise for a healthy heart.
Stop Smoking

A history of smoking is a major link in the relationship between COPD and heart attacks. In fact, people who smoke are up twice as likely to suffer a heart attack compared to non-smokers.
Smoking also leads to high blood pressure and significantly increases your risk for cardiovascular disease. It also affects the balance of cholesterol in your blood and causes plaque to build up in your arteries.
That's not even mentioning the devastating effect that smoking has on your lungs, especially when you already suffer from COPD. Smoking will worsen your symptoms, increase your risk of having COPD exacerbations, and lead to quicker lung function decline.
If you need help to quit smoking, talk to your doctor about quit-smoking medications or programs in your area. You can also visit the CDC's website for a variety of quit-smoking materials and links to smoking cessation guides from the American Lung Association, American Heart Association, and the American Cancer Society.
Prevent COPD Exacerbations

Exacerbations are a major cause of heart attacks in people with the COPD. In fact, experiencing an exacerbation can significantly increase your risk of a heart attack for days or even weeks after after you recover.
One study showed that a patient's heart attack risk is more than doubled for up to five days after an exacerbation. This likely happens because exacerbations cause an increase in a variety of COPD symptoms responsible for putting extra strain on the heart.
Increased respiratory symptoms experienced during an exacerbation, like worsened airway obstruction and shortness of breath, can lead to hypoxemia and put a great deal of pressure on the heart. Exacerbations also tend to increase inflammation in the body, including the blood vessels, which can worsen cardiovascular disease and raises your risk of heart attack.
Exacerbations are also very difficult to recover from, and in some cases results result in a permanent worsening of COPD symptoms. This is bad for both your heart and lungs. By reducing the number of exacerbations you experience, you may be able to preserve your lung function longer and prevent permanent increases in the level of strain that the disease puts on your heart.
Other studies have shown that respiratory infections can increase heart attack risk even in people who don't have COPD. One study found that people who have experienced heart attacks in the past are up to seventeen times more likely to have a heart attack within a week following recovery from a respiratory infection.
This shows how serious of an effect respiratory problems can have on the heart in the short term, and highlights why it's so important for people with COPD to minimize their symptoms and avoid getting sick. Even a minor respiratory illness can cause exacerbations and make COPD symptoms much worse, which can quickly lead to life-threatening events like respiratory failure or a heart attack.
Exacerbations are usually caused by respiratory illnesses and infections, but they can also be caused by exposure to respiratory irritants like allergens and air pollution.

Here are some more tips for preventing COPD exacerbations and heart attacks:
- Too much mucus in your lungs and airways can trap bacteria and cause you to get sick. To prevent mucus build-up and reduce airway obstruction, use airway clearance techniques to move the mucus up and out of your lungs and airways.
- Avoid spending time with or near anyone who is sick, including children. Whenever possible, stay away from sick people's homes and belongings until they have fully recovered.
- Protect yourself from germs when you're out in public places. Wash your hands after touching public surfaces and carry hand sanitizer with you for when you can't use a sink.
- Avoid going to crowded places during the winter months when many contagious illnesses spread. Try to schedule visits to museums, convention centers, concerts, and sporting events outside of cold and flu season or go when they are less crowded.
- Protect your lungs from respiratory irritants like pollution, allergens, dust, and mold. They can cause exacerbations, worsen inflammation, and make your symptoms worse.
- Daily symptom management is key for preventing COPD exacerbations. Make sure you follow your COPD treatment plan carefully and take your medications as prescribed every day in order to keep your symptoms under control.
Make Exercise a Priority

Getting regular physical activity every week is an essential part of keeping your heart and cardiovascular system strong. It also helps strengthen your muscles and increase your endurance, which can improve your mobility and allow you to live a fulfilling, active life with COPD.
Exercise strengthens your heart in many ways, including by reducing blood pressure, improving blood circulation, and reducing stress and anxiety. It can also prevent strain on your heart caused by hypoxemia by strengthening your breathing muscles and helping your body use oxygen more efficiently.
The American Heart Association (AHA) recommends that you get at least thirty minutes of exercise five days a week for a healthy heart. It doesn't matter much whether you do thirty minutes all at once, or break it up into a few ten-minute sessions to do throughout the day.
However, getting daily exercise doesn't mean that you have to join a gym or start lifting heavy weights. Even just walking, doing aerobics, or doing basic body weight or chair exercises is usually enough to stay in shape.
The most important thing is to do what you can manage and get moving right away. Even if you can't meet the AHA's guidelines, getting some activity is always better than getting none.
For example, studies show that walking as little as thirty minutes a day can reduce your risk of cardiovascular disease by 18% and reduce your risk of heart attack by 35%. Some studies even show that walking is just as effective as running or jogging for preventing high blood pressure, diabetes, and heart disease.
COPD can make it difficult to exercise, but having the disease makes it more vital than ever to get more physical activity. It's necessary for your lungs, your heart, your overall health, and for maintaining your mobility and quality of life.
If you struggle with exercise because of severe shortness of breath or other COPD symptoms, talk to your doctor for advice. He might be able to recommend activities or exercises classes tailored to your ability level or refer you to a pulmonary rehabilitation class.
Monitor Your Blood Oxygen With a Pulse Oximeter

As we discussed earlier, people with COPD are particularly prone to experiencing hypoxemia, or low oxygen saturation levels in their blood. This happens when your lungs aren't able to absorb enough oxygen, and tends to occur most often during exercise, bouts of breathlessness, exacerbations, and during sleep.
Hypoxemia puts extra strain on both your heart and lungs and can lead to a variety of serious complications over time. That's why many COPD patients use supplemental oxygen; by providing concentrated oxygen to their lungs, it allows them to absorb more oxygen and prevent their blood oxygen saturation levels from falling too low.
One problem with preventing hypoxemia and using supplemental oxygen is that it can be difficult to know when your blood oxygen saturation falls below normal levels. Watching out for the external signs and symptoms of hypoxemia, like breathlessness and fatigue, is important, but they can be difficult to catch, especially if you experience chronic COPD symptoms every day.
Luckily, there's an easy, cheap solution for keeping an eye on your blood oxygen saturation levels and preventing hypoxemia: a home pulse oximeter. It's a small, non-invasive device that can read your blood oxygen levels by shining an infrared light through your skin.
Pulse oximeters are extremely simple to operate and can be used to check your blood oxygen saturation over and over. It takes only a few seconds to take a reading which makes it a great way to monitor yourself for hypoxemia throughout the day, especially when you sleep, exercise, or feel short of breath.
Your pulse oximeter can also help you learn when to use your supplemental oxygen if you've been prescribed oxygen therapy during the day. It can also give you an early warning of severe hypoxia, a medical emergency that occurs when your blood oxygen levels fall so low that it starves your organs of oxygen.
If you suffer from COPD-related heart problems, a home pulse oximeter can be an invaluable tool for monitoring your heart health and preventing heart attacks. By helping you keep your blood oxygen saturation at a healthy level and warning you when it drops too low, having a personal pulse oximeter could even save your life.
Pulmonary Rehabilitation

Pulmonary rehabilitation is a type of special class designed specifically for people who have COPD and other respiratory diseases. It's a solution recommended often to patients who struggle with a variety of aspects related to their health and managing COPD, including those struggling with heart problems.
Pulmonary rehabilitation is one of the best ways to learn all about how to manage your symptoms and overcome all the different challenges of living with COPD. It's kind of like a variety show that covers all kinds of different, yet related, topics, except each class focuses on a different aspect of living with a respiratory disease.
Through pulmonary rehabilitation, you can practice and build up the skills that can help you keep your heart strong and prevent other COPD complications. Most courses cover most or all of the techniques for heart health that we will discussed in this article, including exercise, breathing techniques, stress management strategies, and proper medication use.
Pulmonary rehabilitation also helps you build the skills needed to keep your heart healthy and stave off COPD-related heart complications like heart attacks and cardiovascular disease. In fact, pulmonary rehabilitation is often referred to as “cardiac and pulmonary rehabilitation” and is often recommended to people who have suffered cardiac events like heart attacks or heart failure.
Attending a pulmonary rehabilitation class is also great opportunity to learn from and ask questions to a variety of medical professionals who are knowledgeable about COPD. You'll also get to meet other COPD patients and the chance to get social and emotional support from your peers.
If you have trouble managing your disease or suffer from COPD-related heart problems, talk to your doctor about enrolling in pulmonary rehabilitation. You will need a referral from your doctor since classes are often in high demand and can sometimes be difficult to get into.
Eat a Heart-Healthy Diet

If you have COPD, it's very important to give your body the fuel it needs to keep your lungs, heart, and muscles healthy. That means getting enough of the right nutrients and avoiding unhealthy sugars, fats, and salt.
Eating an unhealthy diet can take a particularly hard toll on your heart, leading to clogged arteries, high blood pressure, diabetes, and heart disease. All of these conditions strain your heart and can significantly increase your chance of having a heart attack.
LDL cholesterol (or “bad” cholesterol), in particular, is bad for your heart and can cause plaque to clog your arteries, leading to high blood pressure and heart disease. Reducing the amount of saturated fats and trans fats you eat, which are commonly found in meats, dairy, and fried foods, can protect your cardiovascular system by keeping your LDL cholesterol low.
Salty foods can also hurt your cardiovascular system by raising your blood pressure and straining your heart, which can cause heart disease and heart attacks over time. That's why it's so important to limit the amount of sodium in your diet, especially by avoiding soda and processed foods.
Your diet is also an essential part of managing a healthy weight, which is very important for your heart. Being overweight or obese puts an enormous amount of strain on your heart, which is even more dangerous when you also have COPD.
COPD patients who are overweight suffer from worsened shortness of breath, less ability to exercise, and tend to live more sedentary lifestyles. Being obese also makes you more prone to obstructive sleep apnea, cardiovascular disease, and can increase your chance of having a fatal heart attack by up to sixty percent.

Here are some foods you SHOULD EAT as part of a heart-healthy diet:
- Eat more omega-3 fatty acids, which help control cholesterol levels and are found in oily fish. Salmon, mackerel, tuna, and sardines are especially high in omega-3's.
- Choose unsaturated fats instead of saturated fats whenever possible. Unsaturated fats are liquid at room temperature (e.g. olive oil and vegetable oil) while saturated fats are solid at room temperature (e.g. butter and lard).
- Eat whole foods with healthy fats like nuts and seeds.
- Eat plenty of fruits and vegetables, which are high in heart-healthy fiber, antioxidants, and folate.
- Eat complex carbohydrates, like whole grain oats, breads, and pastas, instead of simple carbohydrates like white bread. This helps control your blood sugar, protecting your blood vessels and reducing your risk of diabetes.
- Make home-cooked meals as often as possible, even if you have to make them ahead and reheat them. When you make food yourself, you can control everything that goes into it, which helps you reduce the amount of unhealthy additives and ingredients in the foods you eat.
Here are some foods you should AVOID for a heart-healthy diet:
- Limit the amount of salty and processed foods you eat.
- Look out for hidden sources of salt, including soda, canned foods, frozen foods, processed snacks, cheese, and chicken broth.
- Avoid processed meats, including bacon, sausage, and deli meats.
- Avoid foods high in sugar, including soda, fruit juices, sweetened snacks, and candy.
- Consume alcohol only in moderation. Heavy or excessive drinking increases your blood pressure and makes you more prone to heart disease and heart attacks.
- Limit the amount of saturated fats in your diet, which are found in fast foods, fried foods, hydrogenated oils, and animal fats. Try to keep saturated fats below seven percent of your total daily calories.

For more information on how to eat a heart-healthy diet, see this guide on the University of Marlyand Medical Center's website.
Manage Stress
COPD can be a difficult disease to cope with, and can cause a lot of emotional strain. Many COPD patients struggle with increased stress and anxiety, which is bad for your heart as well as your overall well-being.
Excessive stress can increase your blood pressure, cause inflammation in your arteries, and increase your risk of developing heart disease and suffering a heart attack. Chronic anxiety is hard on your heart as well; it leads to chronically elevated levels of stress hormones and is associated with an increased risk of blood clots and heart attack as well.

People who are stressed and anxious are also more likely to make unhealthy lifestyle choices that raise their risk of heart disease. Stress can make you more likely to overeat, choose unhealthy foods, give up on exercise, or even fall back on vices like drugs, alcohol, or smoking.
That's why it is important to learn how manage stress and get treatment for anxiety and depression. By reducing your anxiety and stress levels, you can reduce your risk of heart attack and significantly improve your mood and quality of life.
Here are some tips for managing stress and anxiety related to COPD:
- Research shows that journaling can be an extremely effective way to reduce anxiety and cope with stress. It works best if you use treat your journal as a creative, judgement-free zone and dedicate at least a few minutes to writing in it every day.
- If you have trouble relaxing and sleeping at night, try progressive muscle relaxation. It helps you relax your body by tightening and releasing each muscle group until you've released all the tension in your body. See this guide from Anxiety BC to learn how to progressive muscle relaxation yourself.
- Exercise regularly and get at least some physical activity every single day; it will strengthen your heart, condition your lungs, and help you reduce stress and anxiety. See this article from WebMD for information about exercising for a healthy heart.
- Mindfulness meditation has been proven to reduce anxiety, improve sleep, and help you learn to relax. It's a great mental health skill for anyone to have and can help you cope with mental and emotional hardships caused by COPD. If you'd like to give it a try, there are many mindfulness guides available online to help you get started; try these guided meditation resources from UCLA Health.
- If you are suffering from chronic anxiety or depression that you cannot manage on your own, don't give up. Seek help from a mental health professional and ask your family and friends for support. Don't suffer in silence or go untreated; there are many therapy techniques and medications that mental health professionals can use to help.
Keep Your COPD Symptoms Under Control

The more symptoms and airway obstruction you experience on a daily basis, the more likely you are to experience hypoxemia and put extra strain on your heart. That's why managing your symptoms and keeping your breathing under control is such an important part of COPD treatment and is so important for your overall health.
When you reduce obstruction in your airways and keep your COPD symptoms at a minimum, it allows your lungs to function more efficiently and keep your blood oxygen at a healthy level. This, in turn, reduces the amount of strain on your heart and reduces your risk for heart attacks and other heart complications.
Managing your symptoms effectively also helps to prevent COPD flare-ups and exacerbations. This can significantly reduce your chances of having a heart attack, since exacerbations are associated with a two-fold increase in heart attack risk.
Here are some tips and techniques for keeping your COPD symptoms under control.
Practice Mucus Clearance Techniques

Using mucus clearance techniques is an effective way to reduce airway obstruction caused by COPD. It works by helping you remove excess mucus that gets trapped in your lungs and airways, blocking air from flowing through.
Some of the most common mucus clearance techniques include huff coughing, chest and back percussion, and positional drainage. All of these methods help move the mucus up and out of the lungs and into your upper airways, where you can huff or cough it out completely. These techniques are also often used in combination with bronchodilators, which make mucus easier to clear out by relaxing dilating (opening up) your airways.
You can also use specialized devices, like a lung flute or a high-frequency chest wall oscillation vest, that help clear out sticky mucus by using vibrations to dislodge it from your airway walls. To learn more about mucus clearance techniques and equipment, check out our previous article on mucus clearance techniques.
Practice Breathing Techniques
There are several breathing exercises that everyone with COPD should know and practice. They help you manage symptoms like breathlessness by teaching you to control your breathing and by pushing trapped air out of your lungs.
You can use breathing exercises to keep your symptoms under control when exercising, doing household activities, and when experiencing COPD flare-ups and exacerbations. To learn more about breathing techniques and how to do them, see our previous article on COPD breathing techniques.
Take a Pulmonary Rehabilitation Class
Many COPD patients who struggle to manage their symptoms are referred to pulmonary rehabilitation. These classes, which are tailor-made for people who suffer from COPD and other chronic respiratory conditions, will teach you all kinds of practical skills you can use everyday to minimize your COPD symptoms and keep your breathing under control.
Pulmonary rehabilitation also provides opportunities to learn skills for exercise, proper diet, emotional well-being, and much more. See the previous section on pulmonary rehabilitation to learn about it in more detail.
Use Supplemental Oxygen

If you suffer from severe symptoms and hypoxemia, your doctor might prescribe supplemental oxygen to help you manage your COPD. Some people only use supplemental oxygen to help them breathe at night, while others use it to manage breathlessness and respiratory symptoms during the day, too.
If your doctor has prescribed supplemental oxygen therapy as part of your COPD treatment plan, make sure to use your oxygen exactly as directed. If you don't, you risk making your symptoms worse, experiencing hypoxemia, and putting extra strain on your heart and lungs.
Treat Sleep Apnea

Many people who have COPD also suffer from obstructive sleep apnea, a condition that affects your ability to breathe while you sleep. Sleep apnea can be especially dangerous for people with COPD, because it causes lapses in breathing that starves their bodies of oxygen at night.
This nighttime hypoxemia caused by sleep apnea causes increased blood pressure and puts extra strain on your heart and blood vessels. This can increase your risk for hypertension, irregular heart beat, heart attacks, and stroke.
For people with COPD or those who have existing heart problems, sleep apnea is especially damaging to the heart and respiratory system. If you have heart disease or have suffered a heart attack in the past, lapses in breathing caused by sleep apnea can even cause sudden cardiac death.
There are certain risk factors that significantly increase your chances of sleep apnea, including smoking, obesity, alcohol consumption, older age, and narrowed airways caused by genetics or by underlying respiratory disease. If you think you may have sleep apnea, you will need to be evaluated by a doctor and undergo a sleep study for a proper diagnosis.
If you have sleep apnea, you will likely be given a CPAP or BiPAP machine to use at night. These devices blow air into your throat and airways to help keep them open, that way your breathing doesn't become obstructed while you sleep.
It's important to use your BiPAP or CPAP machine every single night to prevent heart strain and reduce your risk of having a heart attack if you have sleep apnea. If you don't adhere to treatment, you will continue to experience dangerous lapses in breathing and drops in blood oxygen saturation at night, which eventually leads to a variety of heart problems and other long-term complications.
Your COPD Treatment Plan is Your Life Line

Everyone who has COPD should have a detailed, personalized treatment plan written for them by their doctor. In fact, it's one of the first things that should happen after anyone gets diagnosed with COPD.
That treatment plan should tell you how much you should exercise, healthy lifestyle changes you should make, and a list of all your medications and when you are supposed to take them. It should also include a COPD action plan to help you evaluate and treat your symptoms daily and know what to do when your symptoms flare up.
This action plan is your life line; it tells you what to do when your symptoms get worse, when you are supposed to use which medications, and tells you how to recognize serious symptoms that require medical attention. That's why you should always have your treatment plan with you and always take care to follow exactly what it says.
Adhering to the treatment plan your doctor gives you is the best way to keep yourself healthy and prevent COPD complications, including heart attack. By keeping your symptoms under control it also reduces your risk of experiencing an exacerbation, which helps protects your heart.


.png)



