.png?width=648&name=27%20(2).png)
Oxygen therapy or supplemental oxygen is the use of oxygen for medical purposes. It’s used by around 1.5 million people in the United States and can alleviate symptoms associated with a variety of respiratory conditions such as chronic obstructive pulmonary disease (COPD), asthma, and cystic fibrosis. Although oxygen therapy is a common medical treatment, there seems to be a lot of confusion around what it is, how it works, and why it’s so important.
In order to help you better understand oxygen therapy, we’re going to take a look at some of the terms associated with it including medical oxygen terminology and medical equipment terminology. Medical terms include any terms associated with diagnosing oxygen issues in the body and oxygen equipment terms focus on the actual equipment and processes used to treat oxygen deficiencies. By doing so, you’ll have a better understanding of how oxygen therapy works and how it can benefit certain people.
In the following post, we’re going to take a look at the most common oxygen therapy terms and clarify any misconceptions that you may have about them. Whether you’ve recently had a blood gas test, been diagnosed with a respiratory disease, or you’re just curious, read on to learn more.
Medical Oxygen Terminology
Oxygen is one of the fundamental building blocks of life. All humans need oxygen to survive and all humans need the right amount of oxygen in order to be healthy. While the average person doesn’t spend their time thinking about their ability to breathe or process oxygen safely and effectively, for others, it’s a matter of life and death.
Underlying conditions like heart defects, lung diseases, or physical injury can cause oxygen deficiency and symptoms like lightheadedness, shortness of breath, and even organ failure. If you’re experiencing any of these symptoms, it’s best to visit a doctor as soon as possible and ask about getting a blood gas test. Let’s take a look at some of the medical terms associated with oxygen.
Oxygen Deficiency
Every time you breathe, oxygen enters your bloodstream and red blood cells transport it throughout the body. This oxygen is used to nourish all organs in the body and perform an important process called metabolism. In a healthy person, blood oxygen levels vary between 75 and 100 millimeters of mercury (mm Hg), but slight variations are usually not a concern.
When your blood oxygen level drops below 60 mm Hg you are considered oxygen deficient, and your doctor will most likely prescribe some type of oxygen therapy to return them to normal levels. You should see a doctor if you experience one or more of the following:
- Shortness of breath while exercising or during sleep
- Lightheadedness
- Weakness throughout the body
- Breathlessness while at rest
Oxygen Saturation
Oxygen saturation, also known as O sats, is a term that refers to the saturation of oxygenated hemoglobin in the blood. Hemoglobin is an iron-rich protein found in red blood cells and each one contains four globular protein subunits which can each carry one oxygen molecule. Because each organ in the body needs a very specific amount of oxygen, hemoglobin plays an important role in regulating oxygen levels and ensuring every cell in the body has the oxygen it needs.
One of the most important things to understand about oxygen saturation is the oxygen-hemoglobin dissociation curve, also known as the oxyhemoglobin dissociation curve. This curve compares the partial pressure of oxygen in the blood to the oxygen saturation level. Partial pressure (PaO2) refers to the actual oxygen content found in arterial blood. It’s a measurement of the pressure that’s exerted on a container wall within a mixture of other gases found in the arteries. Oxygen deficiency, like we discussed above, indicates a low partial pressure of oxygen and is measured in mmHg.

On the other hand, oxygen saturation levels are measured as a percentage. The percentage indicates the amount of hemoglobin (Hgb) binding sites that are carrying oxygen. Partial pressure of oxygen and oxygen saturation levels correlate directly meaning a higher partial pressure will result in a higher oxygen saturation level. If all hemoglobin binding sites are filled, this would result in a saturation of 100%.
When diagnosing the cause of symptoms like lightheadedness and shortness of breath, it’s important for your doctor to understand both the partial pressure of oxygen and your oxygen saturation levels. While partial pressure will give them a more accurate picture of your oxygen levels, oxygen saturation levels can be determined without drawing blood using a device like a pulse oximeter.
Hypoxemia and Hypoxia
Hypoxia and hypoxemia are two terms that are often confused, but it’s important to understand how they differ. Hypoxemia simply refers to low oxygen levels within the blood. Respiratory conditions like chronic obstructive pulmonary disease (COPD), pneumonia, or asthma are usually the cause of low oxygen levels, however, other risk factors include old age, smoking, and being at a high altitude. Typically, anything below 60 mmHg is a cause for concern, but your doctor may take action before that.

Hypoxia is similar to hypoxemia but instead refers to low oxygen levels in the tissues of your body. Hypoxia is sometimes, but not always, associated with hypoxemia. If hypoxemia is present, you will likely have lower oxygen levels in various tissues throughout the body. However, hypoxia can also be local meaning it’s only present in a certain tissue. This can result from low hemoglobin concentration (anemic hypoxia), low hemoglobin saturation (hypoxic hypoxia), or poor cardiac output (stagnant hypoxia).
While hypoxia is a partial obstruction of oxygen supply to a tissue, anoxia refers to a complete lack of oxygen in a tissue. This is usually caused by an injury that prevents blood flow like a hypoxic-anoxic brain injury. This type of hypoxia often results in permanent brain injury or death if they aren’t treated quickly and accordingly.
Oxygen toxicity (hyperoxia)
Around 21 percent of the air that we breathe is oxygen. The rest of the air is made up of about 78 percent nitrogen, as well as carbon dioxide, and a small amount of other gases. Because oxygen is such a crucial element for our bodies, you would think that breathing pure oxygen would be healthy, but this is not the case.
While hyperoxia is much more rare than hypoxemia, it’s still possible to have too much oxygen in the body. Oxygen toxicity is divided into two groups: acute toxicity and chronic toxicity. Acute toxicity can damage the central nervous system while chronic toxicity can lead to pulmonary edema, atelectasis, or lung passageway obstruction. Chronic oxygen toxicity has also been found to have an effect on the eyes, mainly in the form of retina damage.

Fortunately, it’s extremely uncommon to experience oxygen toxicity. Most cases of the condition involve divers because diving tanks deliver oxygen at a higher pressure than on land and often use special gas blends like enriched air nitrox. Although it is possible to experience chronic oxygen toxicity while on oxygen therapy, following your doctor’s instructions will ensure that you never get more oxygen than you need.
Cyanosis
Cyanosis is the discoloration of skin, usually on the hands or feet, due to low oxygen levels. The discoloration usually occurs at extremities because oxygen needs to travel the farthest to reach those points. It can result from things like low blood pressure when there is not enough pressure for blood to reach certain parts of the body or artery problems like clots, peripheral vascular disease, or venous insufficiency.
Medication and oxygen therapy are typically prescribed to treat cyanosis, but it will depend on what is causing the issue. For example, if it’s the result of blood clots, you may need blood thinners or other medications. However, if it’s due to a pulmonary issue, you may be prescribed medical oxygen.
Pulse Oximetry
Pulse oximetry is the simplest and least intrusive way to test your blood oxygen. A pulse oximeter device is usually attached to the finger and measures the level of oxyhemoglobin and deoxygenated hemoglobin in the arteries. Because deoxygenated blood is darker, it absorbs more light and because oxygenated blood is lighter, it reflects more light. Your pulse oximeter will compare these two values and give you a general idea of your oxygen saturation.

The benefit of pulse oximeters is that they’re portable and can be used wherever you need them. If you’re currently undergoing oxygen therapy, you should check your oxygen levels with a pulse oximeter regularly to ensure you’re maintaining healthy levels. However, pulse oximetry has limited uses. While your doctor will likely advise you to use one if you have low blood oxygen levels, he/she won’t use it to diagnose any medical condition.
Arterial Blood Gas Test
Arterial blood gas tests (ABG) are another common way of testing oxygen levels in the blood. While ABG tests are more intrusive than pulse oximetry, they provide your doctor with more accurate and detailed information about your health. Your doctor may recommend having an ABG test if you are experiencing nausea, difficulty breathing, shortness of breath, or they have reason to believe that you may have a lung or kidney disease.

During a blood gas test, your doctor will collect a small sample of blood. This blood will usually be drawn from the arm, wrist, or groin using a small needle. Since blood needs to be tested within 10 minutes of being drawn, you’ll get your results shortly after. There are several pieces of information that can be drawn from your arterial blood gas test including:
Partial Pressure of Oxygen / Carbon Dioxide
This is a measurement of the pressure of oxygen or carbon dioxide that’s dissolved in the blood. This will tell your doctor how efficiently your body is able to bring oxygen into the bloodstream and remove carbon dioxide.
Oxygen Saturation
This result will reveal how much oxygen is being carried by the hemoglobin proteins in your bloodstream. Typically, blood saturation levels between 95 and 100 are healthy, and anything below 90 is a cause for concern.
Arterial Blood pH 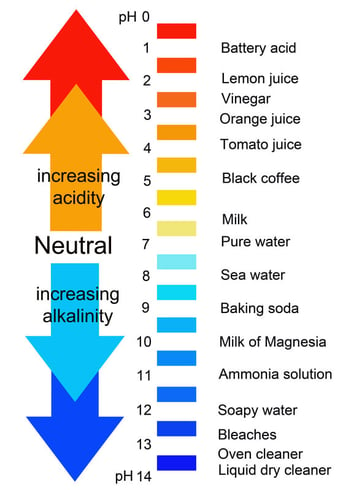
The arterial blood pH level will tell you the amount of hydrogen ions in your blood. Any pH lower than 7.0 is considered acidic while anything higher than 7.0 is considered acidic. A high pH score usually correlates with a higher bicarbonate level while a low pH level is associated with high carbon dioxide levels.
Bicarbonate
Bicarbonate is produced through your body’s metabolic process. It regulates pH levels in your body and then it is transported back to the lungs to be released as carbon dioxide. Low bicarbonate may cause a condition called metabolic acidosis resulting in high blood acidity and high bicarbonate may be a sign of metabolic alkalosis which causes pH to increase in tissue.
Oxygen Equipment Terminology
Oxygen equipment is any equipment used to administer medical oxygen. If your doctor prescribes you oxygen, you will have several options regarding the device and accessories that you use. However, it’s important that you follow your doctor’s directions carefully. Not all oxygen therapy devices are created equal, so you should take your time and ensure that all your needs are met before investing in anything.
Like any industry, the supplemental oxygen industry is constantly evolving and adapting to patients needs. There are hundreds of conditions and diseases that can result in low blood oxygen do everyone has unique circumstances. Let’s take a look at some of the most common oxygen equipment terminology you should be aware of.
Oxygen Tanks

Oxygen tanks are the most standard form of oxygen therapy. The oxygen that it dispenses is compressed and contained within the tank. When it runs out, you’ll need to either get it refilled by a professional or have it swapped out with another one that’s full. Most oxygen tanks are bulky and can’t be moved but you can buy portable ones that are a bit more manageable. However, the more lightweight and portable you oxygen tank is, the less oxygen you will get out of it.
One of the major downsides to using oxygen tanks for oxygen therapy is that they can be very dangerous. First and foremost, oxygen tanks present a major fire hazard. While the oxygen itself is not flammable, oxygen-rich environments can cause some materials to burn that wouldn’t normally burn and can make some things burn more than they normally would. Also, due to the size and material that oxygen tanks are made out of, they can cause injury fairly easily.
Liquid Oxygen Tanks
Liquid oxygen differs from regular oxygen tanks in that they are stored as a liquid rather than compressed air. According to the Lung Institute, liquid gas that’s converted to a gas expands 860 times meaning liquid oxygen tanks are much more compact than compressed oxygen tanks. This also means liquid oxygen is stored at a much lower pressure making it safer to use. The one downside is that it can be more pricey than traditional oxygen tanks due to the process of producing and storing it.
Oxygen Conserver Device (OCD)
An oxygen conserver, not to be confused with an oxygen concentrator is a device that attaches to an oxygen tank and manages its flow type. It’s called a conserver because it causes the oxygen to only be released when the patient inhales, thus conserving a significant amount of oxygen and allowing you to be out and about longer without having to refill your tank. A normal breathing pattern means inhaling one third of the time while exhaling the other two thirds, so oxygen conservers can be extremely effective.

Fixed-Pulse and Demand-Pulse
There are two different types of oxygen conservers: fixed-pulse and demand-pulse. A fixed-pulse conserver has a set volume of air that’s released when a patient inhales. This type of conserver is designed to release a fraction of inspired oxygen (FiO2) comparable to that of a continuous flow device.
Demand-pulse conservers are similar to fixed-pulse units in that they release oxygen when the patient inhales. However, these devices continue to release a set amount of oxygen after the initial volume is released. This could be a consistent flow or it could diminish until the valve completely closes.
Oxygen Concentrators
Oxygen concentrators are some of the most state-of-the-art oxygen therapy devices on the market. As opposed to oxygen tanks, oxygen concentrators don’t actually hold oxygen inside the unit; the oxygen is drawn from ambient air, purified and released in a concentrated form. The obvious benefit to this is that there is never a need to replace oxygen tanks or have them refilled.

There are two types of oxygen concentrators: home oxygen concentrators and portable oxygen concentrators. Home oxygen concentrators can be plugged into any wall outlet while portable concentrators use batteries. And because oxygen concentrators are powered by electricity, accessories similar to those on oxygen tanks are already built in to your device. For example, you can purchase either a continuous flow oxygen concentrator or a pulse-flow oxygen concentrator.
Pulse Flow vs Continuous Flow
Flow settings on oxygen concentrators work similar to conservers that you can buy for your oxygen tank. Continuous flow puts out a constant stream of oxygen and doesn’t account for the user’s breathing rate, whereas a pulse flow or pulse dose oxygen concentrator puts out a set amount of oxygen when the user inhales.
Liter Flow Settings
Another aspect of oxygen concentrators is the liter flow setting. Oxygen concentrators and portable oxygen concentrators can have up to six liter flow settings which determine how much oxygen is actually coming out of the device. While it may seem like the higher setting, the better, you need to follow your doctor’s prescription exactly. Luckily, with a home or portable oxygen concentrator, you can change the liter flow setting with the simple touch of a button. Portable oxygen concentrators range from 3 liters per minute (LPM) to 6 liters per minute. Home oxygen concentrators range from 5 LPM to 10 LPM.
Humidifier

A humidifier is a device that can be attached to many different types of oxygen concentrators, oxygen tanks, and even CPAP devices. If you experience irritation in the nasal passage while using medical oxygen, humidifiers will help prevent this and ensure that you’re breathing humidified air. You will, however, need to replace water in the humidifier when it runs out.
Cannula
A cannula is a plastic tube that delivers medical oxygen to a patient. One end attaches to your oxygen concentrator and the other has two prongs that are inserted into the nose. Because comfort is a major concern when it comes to oxygen therapy, there are a variety of cannulas on the market to help you find one that works best for you. Oxygen cannulas include but are not limited to:
- Curved prong cannulas
- Flared prong cannulas
- Straight prong cannulas
Nebulizer
Although nebulizers aren’t technically “oxygen therapy,” they are part of what’s called “inhalation therapy.” Nebulizers work by using oxygen, compressed air, and a medical solution to create an aerosol, or a mixture of gas and liquid particles. While nebulizers can be used to treat conditions like asthma and COPD, they typically aren’t used to treat low blood oxygen levels like oxygen therapy does.
Recreational vs Medical Oxygen
One common point of confusion for someone that’s new to medical oxygen is understanding the difference between medical and recreational oxygen. Simply put, medical oxygen is used to treat low blood oxygen levels and diseases like COPD and asthma, whereas recreational oxygen is used to improve athletic performance. Many people use oxygen canisters if they're climbing or hiking at high altitude where the air is thin and there's very little oxygen.

Durable Medical Equipment (DME)
If you want to seek compensation from a private health insurance company or Medicare, you should understand the term “durable medical equipment.” Usually what this refers to is any equipment that can withstand repeated use, serves a medical purpose, and is not useful to someone without an illness. If there is any confusion about this, you should clarify with your insurance company.
Conclusion
Oxygen therapy is something that’s constantly evolving so it’s not uncommon for someone to be confused about how it works or why it’s important. Hopefully, this list helps to clarify any confusion about terms or concepts that you may have had and if not, be sure to check back regularly as we’ll upgrade it regularly with any new terms you should know.
If you just started oxygen therapy, your doctor will be your best resource for any concerns you have about oxygen devices, flow settings, and oxygen accessories. While oxygen therapy is becoming safer and easier to use by the year, you will still want to make sure you’re receiving the optimal treatment for your medical condition.


.png)




