If you have COPD, then you know that it can be dangerous when your symptoms suddenly get worse. That's why preventing flare-ups and exacerbations is one of the main goals of treatment for people with COPD.
A COPD exacerbation (also known as an acute exacerbation) happens when you get sick or your lungs get especially inflamed, making your symptoms much worse for an extended period of time. Even though they go away eventually, exacerbations can cause serious health complications and permanent damage to your lungs.
When you have COPD, your quality of life depends greatly on how much you prioritize your health and avoid habits and environments that put your lungs at risk. That means doing everything you can to keep your body strong and prevent acute exacerbations.
In this article we're going to help you do just that by explaining a variety of ways you can reduce your risk of experiencing a COPD exacerbation. We'll help you understand why exacerbations happen, how to recognize the warning signs.
Most importantly, we'll show you a variety of practical methods and techniques you can start using today to avoid flare-ups and exacerbations in the future. So if you're ready to improve your quality of life and take charge of your health today, continue reading for 15 practical ways you can reduce your risk for acute COPD exacerbations.
What is a COPD Exacerbation?
Most COPD patients are able to keep their symptoms under control most of the time, but flare-ups and exacerbations are always a threat. The frequency of exacerbations varies from patient to patient and depends on a variety of risk factors, including age, disease severity, and physical activity level.
On average, COPD patients experience at least one or two exacerbations every year. This does not include minor flare-ups, which might happen much more frequently in response to mild irritants.
Flare-ups Versus Exacerbations
A COPD flare-up is a temporary increase in symptoms that can happen when you breathe in respiratory irritants like dust, smoke, or dry air. Flare-ups are generally mild, short-lived, and treatable at home.
Exacerbations, on the other hand, last longer and are more serious than mild flare-ups. They usually happen as a result of a respiratory illness or infection that causes inflammation, excess mucus, and reduced lung function.
Exacerbations often require a trip to the doctor, although they can sometimes be treated at home. It's important to talk to your doctor about what you should do in the case of an exacerbation and how long you should wait to call your doctor when your symptoms start to get worse.
In general, it's safest to talk your doctor as early as possible if you think you might be experiencing an exacerbation. That's why it's very important to recognize the early symptoms and warning signs of an oncoming acute exacerbation.
Unlike flare-ups, exacerbations can have extended or even permanent effects. Sometimes, even once an exacerbation passes, the COPD symptoms don't improve all the way. Some patient's conditions don't ever get back to the baseline that they were at before the exacerbation, and they have to cope with a minor, yet permanent, increase in symptoms from that point on.
Exacerbations can be life-threatening at any stage of the disease, but they are particularly dangerous for people with advanced COPD. Flare-ups are common in all COPD patients, although sensitivity to respiratory irritants and the severity of the flare-up can range significantly depending on the patient's physical condition and disease stage.
How to Recognize an Exacerbation

Exacerbations are serious business, and recognizing the early symptoms could save your life. An exacerbation can be debilitating, life-threatening, and is are not something you should ever take lightly. Most researchers agree that preventing exacerbations is one of the most important things you can do to live longer and slow down the progression of COPD.
Some exacerbations are mild, but some are serious and require early and immediate treatment to prevent serious complications. Severe exacerbations can cause you to be hospitalized or even end in death.
That's why it's vital to pay attention to how you feel and be able to recognize the early warning signs of an acute exacerbation. You should always be monitoring your symptoms and looking for signs that indicate they're getting worse. Often, the only early warning sign of an exacerbation is a worsening of the symptoms you already have.
If your worsened symptoms don't start to get better soon, you should talk to your doctor right away and begin any additional medication
or therapies that your doctor recommends. The earlier you begin treating an acute COPD exacerbation, the better your chances of avoiding life-threatening symptoms and hospitalization.

If you ignore worsened symptoms, they're likely to continue getting worse. The longer you wait to seek help, the more you'll be at risk for serious complications and the less likely you'll be to make a full recovery.
Here are some of the early warning signs of a COPD exacerbation:
- Rapid, shallow breathing
- More difficulty catching your breath than usual
- More coughing or wheezing than usual
- A change in mucus color (yellow, green, or blood-tinged in color)
- Increased mucus in your lungs and airways
- Feeling unusually sleepy or fatigued
- Difficulty sleeping because your symptoms keep you up
- Having less energy than usual to do normal daily activities
- Breathlessness and fatigue at rest or after extremely light activities
- Confusion
If you think you're experiencing the early symptoms of an exacerbation, follow your COPD treatment plan and talk to your doctor as soon as possible. If your symptoms get significantly worse or you can't catch your breath, seek emergency medical care immediately.
There are certain symptoms that are a sign of serious oxygen deprivation and require immediate medical care. If you experience confusion, a severe headache, difficulty catching your breath at rest, a bluish tint to your skin, or have a sudden difficulty walking short distances, you should seek emergency medical attention immediately.
What Happens When You Have an Exacerbation?
When you have an exacerbation you'll experience increased symptoms and increased mucus production that makes it more difficult than usual to breathe. This happens because of inflammation that reduces your lung function and causes inflammation in your lungs and airways.
Mild exacerbations can sometimes be treated at home, although you should always talk to your doctor about when you should call him first. Your doctor might recommend a variety of medications to use in the short term to manage your symptoms until the exacerbation passes.
Here are some common medications used to treat exacerbations at home:
- Bronchodilator Inhalers: Your doctor might recommend that you use your bronchodilator medication more often or prescribe you a different inhaled medication than you usually use. This will help open up your airways and make it easier to breathe.
- Corticosteroid Medications: Inhaled or oral corticosteroids are common treatments for COPD exacerbations. They help reduce inflammation in your lungs, reduce swelling, and open up narrowed airways.
- Antibiotics: If a bacterial infection is the cause behind your exacerbation, your doctor might prescribe a course of antibiotics to treat it.
However, if an exacerbation gets worse, you might need to go see your doctor or be hospitalized if it gets severe. You should seek emergency medical care if you experience unusually severe symptoms, can't catch your breath, or show signs of low blood oxygen (like confusion, a severe headache, a bluish color to your skin, or extreme fatigue).
If admitted to a hospital, you will receive more intensive treatment that may include bronchodilators, systemic corticosteroids, supplemental oxygen, and breathing support. If your lungs aren't working well enough on their own, you may have to use a ventilator or a positive expiratory pressure (PEP) device to keep your airways open.

Without prompt medical treatment (and even with it), a serious exacerbation can be life-threatening. That's why preventing exacerbations is one of the most important things you can do to stay healthy and live longer with COPD.
What Causes COPD Exacerbations?
|
|
| Photo by Senior Airman Anthony Sanchelli |
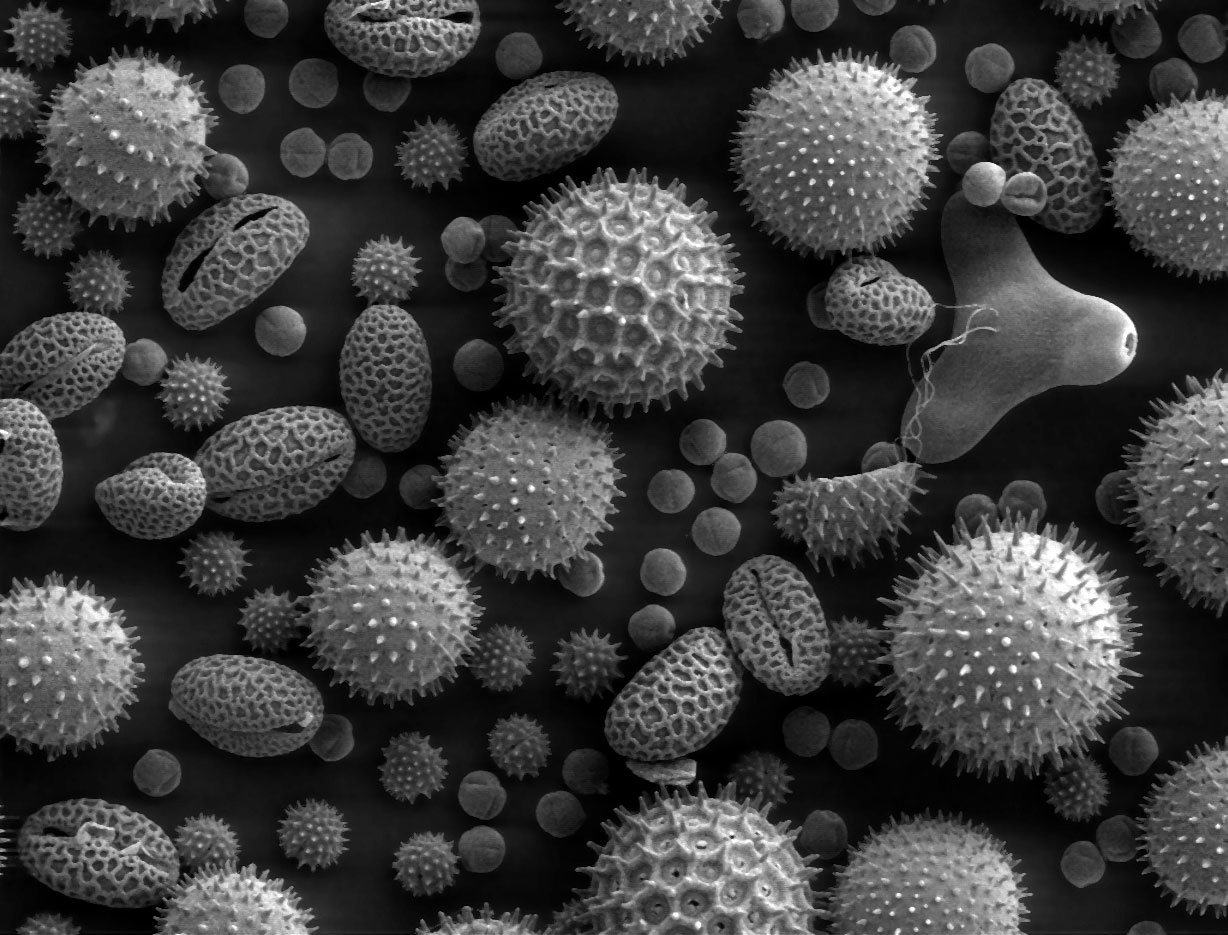
There are many different COPD triggers, including dust, pollen, and cold air, that can cause your symptoms to get worse. However, these irritants usually only cause minor flare-ups, not full-blown exacerbations.
However, exposure to COPD triggers like respiratory irritants can significantly raise The majority of the time, exacerbations are caused by a respiratory illnesses or infection, not respiratory irritation alone.your risk of subsequent exacerbations.
According to research, respiratory illnesses cause 70 to 80 percent of exacerbations experienced by people with COPD. That's why it's so important to do whatever you can to avoid getting sick, including getting vaccinations, practicing good hygiene, and living a healthy lifestyle.
Here is a list of some of the most common causes of COPD exacerbations:
- Pneumonia
- The flu
- Seasonal allergens
- Smoke
- Air pollution
Unfortunately, in up to one-third of cases doctors are unable to determine the cause of a COPD exacerbation. It's important to make choices that limit your risk of having an exacerbation, but there's no way to reduce that risk to zero.
There are certain risk factors for exacerbations that you have little or no control over, like your age and the severity of your disease. Here are some common factors that put you a greater risk for exacerbations if you have COPD:
- A history of frequent exacerbations
- If you've had an exacerbation within the past year
- If you have more severe COPD symptoms (e.g. a severe daily cough or severe breathlessness every day)
- You have severely reduced lung function
- Low BMI
- Lack of exercise
- Old age

Taking care to avoid exacerbations is one of the most important things you can do to stay healthy, stay strong, and maintain your quality of life while living with COPD.. If you are ready to learn what you can do to protect your lungs and maintain your quality of life, continue reading to learn about fifteen different ways to avoid COPD flare-ups and exacerbations.
How to Prevent a COPD Exacerbation
Now that you understand the risk factors for exacerbations, why exacerbations happen, and how to recognize the early warning signs, it's time to learn how to prevent them. Even though you can't always avoid exacerbations, there are many different things you can do in your daily life that reduce your risk.
In these next sections, we're going to show you how you can avoid exacerbations by incorporating simple habits and techniques into your everyday life. We'll go in-depth into a variety of activities, useful techniques, and special precautions you can take to reduce your risk.
Don't put it off any longer; continue reading to learn about a variety of practical steps you can take today to reduce your risk of experiencing a COPD exacerbation.
Avoid Weather and Temperature Extremes
Hospitalizations for COPD-related exacerbations and complications go up significantly in extreme temperatures and weather. That's why you have to be particularly careful to protect yourself during the summer and winter months.
In general, it's a good idea to avoid going outdoors whenever it is extremely hot or cold outside. Both hot and warm air are hard on your lungs, make it difficult to breathe, and can make you more prone to flare-ups and exacerbations.
Avoiding Hot Weather

For some people with COPD, the summer heat brings relief and decreases their symptoms. But for those who are not so lucky, the hot air can make a variety of COPD symptoms worse.
When you spend time in the heat, it raises your body temperature, which makes your body have to work harder to cool you down. This is taxing on your lungs, which already need extra energy to function, and can make it much more difficult to breathe.
You are also more likely to get dehydrated and feel fatigued when you are out in the hot, humid air. Hot weather also tends to correspond with higher ozone pollution levels, which can irritate your lungs and make you even more prone to flare-ups and exacerbations.
Here are some tips for staying healthy and avoiding exacerbations in hot weather:
- Always stay indoors when it is very hot or the air quality is low. Plan exercise and outdoor activities for milder days.
- Plan activities during the early morning or early evening, when the temperatures are cooler. The hottest temperatures tend to occur between 11 am and 3 pm every day.
- Drink lots of water during the summer, especially when you exercise or spend time outdoors. Always bring a bottle of water with you when you go out.
- Keep your home cool and air-conditioned. If you don't have air conditioning, go to a public place that does have AC, like the library or mall, on very hot days.
- If you feel overheated, try taking a cool bath or shower to cool down.
- Use a fan in your bedroom at night or any other rooms that tend to get hot and stuffy. You can also get a hand-held, battery-powered fan to bring with you whenever you go outdoors in the heat.
- Drink a sports drink or salty food after sweating or spending time in the heat to replenish lost electrolytes.
- If you are sensitive to allergens, always check your local pollen and allergen forecast. You can check it online at pollen.com.
- Bring your inhaler and any quick-relief medications with you whenever you go out in case your symptoms flare up.
Avoiding Cold Weather

Cold weather can also make COPD worse and put you at a much greater risk for exacerbations. In fact, one study showed that cold weather caused a significant increase in hospital admissions, with up to a 20% increase in hospitalizations for people with COPD. The main factors increasing the risk were lower temperatures, windchill, cold weather that lasted for more than a week.
Winter weather causes an increase in symptoms in part because cold air is denser, drier, and more difficult to breathe. Cold, dry air dries out your airways and nasal passages, causing inflammation that worsens symptoms and increases mucus production.
Together, these effects make it more difficult to breathe and increase your risk of getting an illness or infection. The effects are the worst at temperatures below freezing, but COPD hospitalizations increase at temperatures as high as 41 degrees Fahrenheit.
That's why it's so important to stay indoors and take extra precautions during the winter months. Here are some tips for avoiding cold weather and staying healthy during the winter:
- Stay indoors on cold days and when the air quality is low. Don't exercise or do other physical activities outdoors; instead plan them for warmer days or save them for a warmer season.
- Always dress warm for cold weather and use layers so you can add or remove them if your comfort level changes.
- Always breathe through your nose, not your mouth. This allows the air to warm up and pick up moisture as it travels through your airways to your lungs.
- Cover your mouth with a scarf or cold weather mask anytime you have to be out in the cold air. This traps the heat and moisture from your breath in order to warm and humidify the air you breathe.
- If you use supplemental oxygen, cover your oxygen tank and tubing when you go outdoors. You can string your tubing underneath your jacket or coat to keep it warm.
Humidity

Humidity is yet another weather condition that can have a significant effect on people with COPD. Most people do best when the humidity is around 40 percent, and a humidity range between 30 and 50 percent is recommended for people with respiratory conditions and diseases.
Both too little and too much humidity makes it difficult to breathe and can make your COPD symptoms worse. Dry air is harsh and irritating to your lungs, while extra-humid air is heavy and hard to inhale.
Humidity tends to be highest in warm weather, because warm air is able to hold more moisture. The air tends to be much drier during the winter, and the dense, cold air tends to make air pollution worse as well.
But humidity isn't just about the weather; even if the humidity is ideal outdoors, the humidity inside your house can still get high. Running a shower or bath and using appliances like your dishwasher or washing machine can raise the humidity in your home if you're not careful.
Humidity effects everyone differently, so pay attention to what humidity levels make your symptoms better or worse. To reduce your chances of flare-ups and exacerbations, you should avoid spending time outdoors any time the air is especially humid, especially dry, or polluted.

Here are some general tips for dealing with dry and humid weather:
- Get a humidifier for your home and use it during the dry winter months. You can get one for your bedroom and any other space you tend to spend a lot of time in, or you can get a whole-house humidifier that hooks up to your home's main ventilation system.
- When the humidity outdoors is very high, keep your windows and doors closed to keep the moist air out of your home.
- Make sure any appliances that release moisture into the air, including your washing machine, clothes dryer, stove, and dishwasher well-ventilated.
- Whenever you take a shower or bath be sure to open a window or turn on your bathroom fan to vent extra humidity.
- Use the vent fan on your stove when cooking steamy or smoky foods.
Attend Pulmonary Rehabilitation
Getting exercise and living an active life is another one of the best things you can do to keep your body healthy, strengthen your breathing muscles, and reduce your risk of COPD exacerbations. But in order to get enough exercise, you need to know how to manage your symptoms and control your breathing while you work out.
That's why many doctors recommend that COPD patents attend pulmonary rehabilitation, a special class designed specifically to help people with respiratory diseases live healthier, happier lives. Many people begin pulmonary rehabilitation after they have difficulty exercising and managing their disease on their own.
But pulmonary rehab is about more than just exercise; it's about learning how to manage all the different aspects of your life that are affected by COPD. You'll learn how to keep your lungs healthy, how to manage your symptoms, and how to handle the stress and emotional strain of living with a chronic disease.
Classes are usually run by medical specialists or social workers who have a wealth of knowledge and experience to share. Classes usually focus on these main areas:
- Exercise training classes
- Learning and practicing breathing techniques
- Diet and nutritional counseling
- Lung health and disease education
- Learning how to conserve energy for what's most important
- Mental health counseling and group support sessions
- Learning how to use oxygen and other medications to manage respiratory symptoms
Research shows that taking a pulmonary rehabilitation class increases exercise capacity and overall health in people with COPD. Multiple studies have also found that pulmonary rehab significantly reduces patients' risk of future exacerbations and hospital admissions, too.
Pulmonary rehabilitation is like a crash course on how to live the best possible life while managing your COPD. It's one of the best things you can do to jump-start your COPD treatment and learn how to integrate positive, healthy habits into your everyday life.
Find a Pulmonary Rehabilitation Class Near You

Pulmonary rehabilitation classes vary depending on where you live and what kind of help you need. Some programs are hosted as group classes at hospitals and clinics, some offer individual instruction, and some can even be done partially or fully at home.
If you have COPD, talk to your doctor about whether or not you could benefit from pulmonary rehabilitation. Your doctor can give you a referral and help you find a class in your local area that works for you.
Here are some resources to help you locate a pulmonary rehabilitation program near you:
- See the COPD Foundation's interactive map of pulmonary rehabilitation programs across the United States
- Search a directory of pulmonary rehabilitation centers by state and city at emphysema.net
- Call 1-800-LUNGUSA (1-800-586-4872) to get information on pulmonary rehabilitation classes from the American Lung Association's Lung HelpLine
Check Air Quality Reports
If you've never paid attention to air quality reports before, now is the time to start taking them seriously. Outdoor pollution and allergens are bad for your lungs and increase your risk for exacerbations.
Particles, bacteria, mold, and other airborne contaminates get into your lungs and airways when you breathe, causing inflammation and increased mucus production. These respiratory irritants worsen COPD symptoms, increase your risk for infection, and cause further damage to your lungs over time.
Studies have shown that even short-term exposure to air pollutants significantly increases the risk of exacerbations in people with COPD. Gaseous pollutants like ozone and airborne particles like dust and mold, in particular, carry the highest risk.
Polluted air can affect your health within minutes, hours, or days of exposure. If you have COPD, spending time outdoors in hazardous pollution could give you worsened symptoms for days.
One of the most important ways to protect your lungs is to watch your local air quality reports and know how to protect yourself when pollution and pollen levels are high.
Air Quality Reports

Typical levels of air pollution vary from city to city, but they also vary from day to day. The amount of smog you get exposed to when you go outside depends on the temperature, humidity, weather patterns, traffic, and a variety of other factors.
You should check the air quality every day before you go out and limit the amount of time you spend outside when the air quality is low. Most local weather forecasts include air quality reports, but you can also check your local air quality at airnow.gov.
Use the daily air quality forecasts to plan activities ahead of time, especially for outdoor exercise and other physical activities. If the air quality turns out to be poor, reschedule any activities that require you to spend extended time outdoors for a day when the air will be healthier to breathe.
Another thing to remember is that you should close all of your doors and windows on days when the air quality is low. This will help keep smog and other pollutants out of your home and help keep your indoor air healthy to breathe.
Here's how to read the different levels of your local air quality report:
- AQI 0-50 (green): Good, little or no risk
- AQI 51-100 (yellow): Moderate, could be unhealthy for very sensitive groups (including people with severe COPD)
- AQI 101-150 (orange): Unhealthy for sensitive groups (including people with COPD and other lung conditions)
- AQI 151-200 (red): Unhealthy for everyone, but especially sensitive groups
- AQI 201-300 (purple): Very unhealthy, could trigger serious health effects
- AQI 301-500 (maroon): Hazardous, emergency conditions (such as smoke from a nearby wildfire)
Check Pollen Reports

A large percentage of people with COPD also suffer from allergies to things like mold, pollen, and dust mites. These allergens can cause bronchial spasms and inflammation that make your COPD symptoms worse and put you at risk for an acute exacerbation.
If you have allergies, you should make sure check your local pollen report every day, especially during the spring, summer, and fall. To reduce your risk of an exacerbation, you should always avoid going outdoors on days when pollen and other allergen levels are high.
Other Tips for Avoiding Pollution and Allergens
Checking air and pollen reports are just the first step to protecting yourself from airborne irritants. To really protect your lungs, you'll need to actively avoid places where irritants are present and make an effort to reduce the amount of airborne irritants in your home.
If you are a smoker, the most important thing you can do for your health is to quit smoking altogether. If other people you live with or spend time with smoke, ask them to never smoke around you or your home.
Here are some additional tips for avoiding respiratory irritants in your daily life:
- Always make an effort to stay indoors when the air quality index or pollen levels are high. Reschedule outdoor activities on high-pollution days and try to schedule outings on days when the air quality is good.
- Always keep your inhaler and quick-relief medications with you when you go outside.
- Keep the windows and doors in your home shut tight on days when the pollution and pollen levels are high.
- Keep your home clean; dust, vacuum, and clean your floors and surfaces often to remove dust, pollen, pet dander, and other contaminates.
- Keep your pets off of your furniture and give them regular baths and brushings to keep allergens and pollutants from building up in their fur.
- Keep your windows rolled up to keep city pollution and exhaust fumes out of your car.
- Use the re-circulation option for your car's ventilation system to re-circulate the air in your cabin instead of pulling in polluted air from the road.
- Try to avoid high-traffic roads and drive when the traffic is lighter.
Avoid Common Respiratory Irritants

As we've already mentioned, respiratory irritants like allergens and smog can worsen your respiratory symptoms, damage your lungs, and significantly increase your chances of experiencing an exacerbation. That means that you should be very cautious about the air you breathe and avoid contaminated air as much as possible.
Outdoor smog, smoking, and air pollution are some of the most common sources of exposure to respiratory irritants. If you have allergies, pollen, mold, and dust mites can also inflame your respiratory system.
Here is a list of the most common respiratory irritants that you should avoid:
- Air pollution and smog
- Dust and dust mites
- Pollen
- Mold and mildew
- Smoke
- Cooking fumes
Airborne irritants like the ones on this list get into your lungs and airways when you breathe contaminated air. These irritants are more hazardous for people with COPD because they cause more damage to their already damaged lungs. They can also worsen symptoms, quicken disease progression, and makes exacerbations more likely.
The inflammation that respiratory irritants trigger causes your airways to narrow and increases mucus production that clogs your lungs and airways. This blocks airflow to your lungs which makes it even more difficult to breathe and triggers symptoms like coughing, wheezing, and shortness of breath.
In this way, exposure to airborne irritants weakens your lungs and makes you more likely to experience a COPD exacerbation. Even if the irritants themselves don't trigger an acute exacerbation, the inflammation could increase your risk for infections and further inflammation that leads to an exacerbation later on down the line.
Other Airborne Contaminates to Watch Out For
It's also important to know about some less obvious, often overlooked sources of airborne irritants that many people don't even think of. You should be familiar with every irritant and pollutant that could harm your lungs so you can avoid exposing yourself unintentionally.
Here are some oft-overlooked sources of airborne irritants and pollutants:
- Radon: This is a toxic gas that can be present in the ground around your home. You will have to hire an inspector to check for radon in and near your house to ensure that you're not being exposed.
- All Sources of Smoke: This includes incense, barbecue grills, fireplaces, bonfires, wood-burning stoves, car exhaust, kitchen mishaps, and more.
- Asbestos: Asbestos is a common material used in home insulation, wall paint, tiles, and a variety of other common home materials. If you live in an older house there is a very good chance you have asbestos in your home. If it stays in place it is not very dangerous, but if it gets disturbed and mixed into the air, it can cause serious damage to your lungs. You should always get your house checked for asbestos before doing any home remodeling or renovations.
- Construction Sites: You should avoid going near construction sites because they often produce a lot of pollution and kick up a lot of dust that can be harmful to your lungs. If you live or work near a construction site that you cannot avoid, wear a dust mask or certified N-95 particulate respirator.
Use a Respirator to Protect Your Lungs

If you are very sensitive to airborne particles like dust or mold, you might benefit from wearing a special particle mask that filters these particles out as you breathe. These masks, often called respirators, can come in handy when you clean or might be exposed to hazardous chemicals, dust, or mold.
You should look for certified, consumer-quality N-95 masks, which effectively filter out 95 percent of airborne particles like dust and mold, even particles that are too tiny to see. Make sure sure any mask you get has been certified by the National Institute for Occupational Safety and Health (NIOSH) to ensure quality. You can usually find NIOSH-certified particle masks at hardware and home improvement stores.
Talk to your doctor before getting a respirator because, for some patients with reduced lung function, wearing a particle mask makes it more difficult to breathe. This happens because it takes extra effort to pull air through the mask when you inhale. If you are wearing a respirator, remove it immediately if you notice a headache, nausea, or shortness of breath.
Reduce Indoor Air Pollution

It doesn't do much good to avoid outdoor pollutants by staying indoors if the air inside your home is full of contaminates, too. That's why it's so important to reduce the amount of pollen, mold, dust, and other pollutants that circulate in the air in your house.
Indoor pollutants come from a variety of sources, including pets, household chemicals, in-home appliances, and irritants you track in from outdoors. If you don't make an active effort to get rid of these contaminates regularly, they can build up in the air in your home and cause even further damage to your lungs.
Here are some of the most common sources of indoor air pollution:
- Mold and mildew
- Dust and dust mites
- Chemicals and fragrances (from cleaning products, perfumes, etc.)
- Fumes from washing machines, dishwashers, and stoves
Reducing the amount of respiratory irritants and pollutants inside your home is just as important as avoiding the outdoors on days when the air quality index is high. Read the following sections for a variety of ideas and practical tips for improving the air quality in your home.
Reduce Dust and Pollen
Dust, pollen, and pet dander tend to build up in the little-trafficked places in your home, such as basements, closets, corners, and shelves. When this dust gets kicked up into the air, you breathe it in, where it inflames your lungs and airways and makes your COPD symptoms worse.
This is especially true if you have allergies, and it can significantly raise your risk of experiencing a COPD exacerbation. Here are some general tips for reducing the amount of dust and allergens in your home:
- Check the air ducts in your home at least once a year. If there is visible dust build-up, mold, or you frequently experience worsened respiratory symptoms at home, you should get your air ducts professionally cleaned.
- Get high-quality, hypo-allergenic air filters for your HVAC system and replace them every few months.
- Use a duster or damp towel to clean dust off of counters, shelves, cabinets, and other horizontal surfaces.
- Always take off your shoes immediately after coming indoors to avoid tracking dust, pollen, and other grime around your house.
- Clean up and organize any cluttered areas that gather dust. Consider reducing the number of small, dust-collecting items and decorations you have or relocating them to a closet or cabinet.
- Sweep your floors and vacuum your carpet often to remove dust and other allergens.
- Clean fabrics and plush objects regularly to remove pollen, dust, and other irritating particles. That includes curtains, rugs, couches, carpets, etc.
- Keep your windows and doors closed on days when pollen levels are high to keep allergens out of your house.
- Consider getting hardwood floors or getting rid of decorations like rugs, curtains, and drapes.
- Control the humidity and moisture in your home to reduce dust mites, insects, and mold that cause respiratory symptoms.
- Get an air filter or purifier for your home.
- Wear an N-95 face mask to protect yourself from dust, pollen, pet dander, and hazardous chemicals when you clean.
Control Pollution and Fumes from Home Appliances and Products

A variety of home appliances that you use every day emit fumes that can irritate and damage your lungs. You also have to beware of scented lotions and other products that can trigger COPD symptoms.
Here are some tips and ideas for eliminating noxious fragrances and fumes from your home:
- Open your windows on mild days when the forecast says pollution and pollen levels are low. This will air out your house and exchange stale, polluted indoor air with fresher, cleaner air from outdoors.
- Make sure appliances like your dryer, dishwasher, and stove are properly vented. If you have old appliances, get them inspected to make sure they aren't leaking any pollution into your home.
- Never smoke or allow others to smoke in or around your home.
- Avoid using fireplaces or wood-burning stoves. Even if they're well ventilated they can leak smoke and particles into the air.
- Invest in a HEPA filter or other air purifying device. You can get air purifiers that work for single rooms or whole-house units that filter all the air in your house.
- Don't use lotions, shampoos, or other body products with strong fragrances. Look for unscented products whenever possible, and ask others who live in your home to do the same.
- Replace harsh chemicals and cleaners with milder, natural products instead. Continue reading to learn about how to make your own natural cleaners later in this article.
Control Moisture and Humidity

Too much humidity is bad for your lungs and encourages the growth of bacteria, dust mites, and mold. On the other hand, too little moisture in the air can make it difficult to breathe, too. Luckily, there are lots of tools and techniques you can use to keep the humidity in your home within a comfortable and healthy range.
Controlling leaks and cleaning up spills is particularly important to prevent mold and mildew growth in your house. Moisture from your shower, pipe leaks, water damage, or any other source is nearly guaranteed to grow mold if it stays damp for more than 12-24 hours.
Anytime you have a leak or flood, clean up the water immediately and carefully air out damp items, including the carpet. You should check mold-prone places like your basement, bathrooms, and ceilings regularly for any visible mold or water spots, especially if you've ever had a pipe leak or flood.
It's also important to open a window or turn on your bathroom vent whenever you take a shower or bath. The humidity that builds up from running the hot water can encourage mold growth, make it difficult to breathe, and increase the humidity in your home to uncomfortable levels.
Another common source of moisture is home appliances, including dishwashers, dryers, and stoves. You should always vent these appliances, whether directly through ventilation tubing or by opening up a window or turning on a vent.
Finally, if the air in your home is too dry or too wet, you can get a humidifier or dehumidifier, respectively, to help you better control the moisture in the air. You can get single-room devices or whole-house humidifiers that moisturize your whole home through the main ventilation system.
Here are some additional tips for controlling moisture and humidity in your home:
- Promptly wipe up any water or spills and repair leaky pipes immediately after you notice them.
- Open windows and use fans in your home strategically to pull excess humidity out of your house.
- Running your air conditioning on hot, humid days will dehumidify the air slightly.
- Take shorter showers to reduce the amount of humidity that builds up in your bathroom. Using colder water can help, too.
- Invest in a humidifier for the dry winter months and/or a dehumidifier for the hot, humid months. Ideal humidity levels for most people with COPD fall within the 40 to 50 percent humidity range.
- Check your local weather report daily to see what the humidity level will be. On particularly humid days, keep your windows and doors shut to help keep the moisture out of your home.
- If you have any moldy or water-damaged carpet or furniture, you should get rid of it or have it professionally cleaned.
- Replace and clean moisture-holding items like bath towels, hand towels, and cleaning sponges often to discourage mold growth.
- Check your shower walls, floor, and shower head for mold or mildew regularly.
Keep Your Home Squeaky Clean

In addition to the specific steps you should take to keep the air in your home clean, you'll need to keep up with other forms of household cleaning as well. Doing so will not only reduce your risk of exacerbations, but it will also help you work some extra physical activity into your daily routine.
Thoroughly cleaning all the surfaces in your house removes bacteria, viruses, and other respiratory irritants that cause exacerbations. Keeping your home free from dust, mold, and grime will also help with allergies and prevent minor symptom flare-ups.
But cleaning does come with some hazards, including exposing yourself and your lungs to dangerous household chemicals and dust as you clean. That's why it's important to take precautions and enlist help, especially for heavy cleaning tasks.
In the next sections we're going to show you some new techniques and ideas for tackling different cleaning projects in your home. We'll give you practical ideas to help you tackle everyday tasks and special projects, tips for conserving energy when you clean, and show you ways to avoid using noxious chemicals that could irritate your lungs and airways.
Use Natural Products
Many household chemical sprays and cleaning agents contain noxious chemicals that are bad for your lungs. If you use them to clean, it's very difficult to avoid breathing them in, and if you have to use a lot, the fumes can contaminate an entire room or the air in your whole house.
These irritating fumes can stick around for hours after you clean and irritate your lungs. To avoid hurting your lungs and making your symptoms worse, opt for natural, mild cleaners instead of chemical ones.
What to Use Instead of Harsh Chemicals

You can find all-natural cleaners at many retail stores, but they are often less effective and overpriced. Instead, you can make you own cleaning products at home using readily available supplies.
Many of the following DIY cleaning product “recipes” include vinegar, baking soda, and soap, which are effective cleaning agents that will not irritate or damage your lungs and airways. Some use small amounts of ammonia, which can be irritating, but is safe to use in moderation.
DIY All-purpose Cleaner
- Put ½ cup of baking soda into a large spray bottle.
- Add enough water to cover and dissolve the baking soda.
- Carefully pour 1 cup of vinegar into the spray bottle (The mixture will fizz, so make sure to add it in slowly).
- Fill up the spray bottle the rest of the way with water and let it sit for 8-12 hours, or overnight.
- Shake it lightly to mix, then let it sit until it stops fizzing.
- Now your all-purpose cleaner is ready to use!
- Bonus tip: Add an extra teaspoon of dish detergent to the mixture to give it grease-cutting properties for oily messes and spills.

DIY Window Cleaner
- This cleaning product uses ammonia, so take care when mixing or using this spray. Keep the mixture away from your face, don't breathe in the fumes, and wear a mask, respirator. Better yet, have someone else mix and/or use it for you.
- Pour one cup of vinegar into a large spray bottle.
- Add two cap-fulls (about 6-8 teaspoons) of ammonia to the bottle.
- Shake to mix, and your window cleaner is ready to go!
DIY Toilet Cleaner
- Get two full cups of baking soda and pour them right into the bowl of yo toilet.
- Use a toilet brush to thoroughly scrub the bottom and sides of the bowl.
- Flush the toilet.
- Pour in two cups of vinegar.
- Use a toilet brush to mix in the vinegar and swish it around the bowl.
- Flush again. Now you're done!

DIY Carpet Deodorizer
- Sprinkle a small amount of baking soda over spots on your carpet or upholstered furniture to absorb offensive odors.
- Let it sit for at least 12-24 hours.
- Vacuum up the baking soda, making sure to get all of it up. That's all! Your carpet or furniture should smell much more fresh and clean.
There are certain chemical cleaning products, like bleach, that there's just no replacement for. Just make sure to avoid breathing the fumes whenever you have to use noxious cleaning agents like ammonia or bleach and, if you have one, use a mask or respirator to cover your nose and mouth.
Tips for Everyday Home Maintenance

Next we'll give you a variety of practical tips for making household duties like vacuuming, dusting, and laundry more easy and efficient. Use these techniques to save time, energy, and effort when you clean.
Dusting
- Wear an N-95 respirator to avoid breathing in dust and other airborne particles as you clean (this applies to any kind of cleaning, including vacuuming and cleaning surfaces and floors).
- Get a duster with a long handle to make it easier to reach tall and low places. That way you don't have to bend over often or climb onto chairs to reach all the dust-collecting nooks and crannies in your house.
- Try bringing a stool with you to sit on as you dust. Use it to sit near shelves, cabinets, and other dusty places so you don't have to stand and stoop while you clean.
- Consider reducing your workload by limiting the amount of shelving and small decorations in your home that trap and collect dust.
- Always dust before you vacuum. That way you can immediately vacuum up all the dust and other irritating particles you've knocked off of surfaces in your home.

Vacuuming
- Take rest breaks if you tend to get tired from walking while pushing and pulling the vacuum.
- Practice good posture and don't lean or hunch while you vacuum. This will prevent you from straining your muscles and make it easier to breathe.
- Use the pursed-lips breathing technique to control your breaths.
- Sync up your movements with your breathing to avoid breathlessness while you vacuum. Breathe in as you pull the vacuum toward yourself and breathe out as you push it away.
- Always take care when emptying or disposing of your vacuum bag. Cover the opening with a damp cloth or newspaper to catch dust and other particles and prevent them from dispersing into the air.
Cleaning Floors
- Use the pursed-lips breathing technique to control your breaths and make it easier to breathe.
- Stand up straight and practice good posture to prevent muscle strain and breathlessness.
- Use a broom and mop with long enough handles that you don't have to bend or stoop while using them.
- Similarly, use a long-handled dustpan to avoid bending over when sweeping up.
- Like when you vacuum, sync up your breathing with your movements to make it easier to breathe. Breathe in as you pull the mop toward you and breathe out as you push it forward.

Cleaning Surfaces and Minor Messes
- To avoid having to bend over or get on your knees, use a lightweight mop to clean up minor spots and spills.
- Get a grabber or long tongs to pick items up off of the floor or to retrieve things that get pushed underneath your bed or other furniture.
- When using a spray with chemicals or ammonia, spray the counter or other surface and walk away for a minute or two. This will give the chemicals time to settle and disperse, reducing the amount of noxious particles you might accidentally breathe in.
- Always keep the room that you're cleaning in well ventilated, especially if you are using chemicals or sprays. Open a window or turn on a fan to circulate air in enclosed rooms and spaces.
Laundry
- If you can, get a front-loading washer and dryer. That way you don't have to bend and reach as much when getting things out of the machine.
- Sit on a stool to conserve energy while sorting clothes, folding clothes, or getting them out of the dryer.
- Get a rolling laundry basket to reduce the amount of lifting and carrying you have to do.
- Drop your clothes off at a laundromat. Many offer relatively affordable bulk clothes washing and folding services.
Getting Help

Cleaning and keeping up with housework is a great way to stay active and get some extra physical activity in your day. However, it's important not to push yourself too hard or do activities that expose you to irritants or make your symptoms worse.
If you find your daily cleaning tasks tiring, try taking it slower and spreading out your tasks throughout the day. Put on some music or headphones while you work to reduce the tedium and make cleaning more engaging and fun.
It's a good idea to get help at least occasionally, whether from friends, family, or a professional cleaning service. Depending on your physical condition you might need someone to come once a month or even once a week or more often to help with heavier cleaning tasks.
Avoid Getting Sick
When you have COPD, a flu is more than just a flu. Getting any kind of respiratory virus or infection can wreak havoc on your lungs and cause a life-threatening exacerbation.
That's why it's so important to protect yourself from viruses and bacteria. That means getting vaccinated, staying on top of your medications, and going out of your way to avoid anything that could get you sick.
Get Vaccinated
 |
| Photo by Senior Airman Areca T. Wilson |
One of the most important things you can do to protect yourself from illnesses that cause exacerbations is to get regular vaccinations. Even a mild flu can cause serious complications for people with COPD, even if the symptoms are mild and you are able to keep your symptoms under control.
People with COPD are also much more likely to get pneumonia as the result of a mild flu or other illness. To help prevent exacerbations and other complications, doctors recommend the flu vaccine and Pneumococcal (pneumonia) vaccine for all people with COPD.
You'll need to get a new flu shot every year to protect against that year's most common influenza virus strains. Most adults who are up-to-date with their shots have already received a pneumococcal vaccine, but the CDC recommends getting two more doses if you're over the age of 65.
You can get flu and pneumococcal vaccines from your usual doctor or you can visit a local pharmacy that offers vaccinations.
Getting vaccinated can be very effective at keeping you healthy during peak flu season, but the flu vaccine is not always 100% effective. It's still just as important to practice proper hygiene and protect yourself from germs and people who are sick.
Stay Away from Sick People

Anytime anyone you know is sick with a contagious illness, you should stay away from them at all costs. Even minor colds and non-respiratory illnesses can compromise your lungs and immune system and cause an exacerbation.
People with COPD tend to have compromised immune systems, which is part of the reason minor illnesses can have such dangerous effects. But it also means that you are much more prone to contracting contagious illnesses, and more prone to getting secondary infections, too.
It's always disappointing to have to cancel a get-together or an evening out with friends, but it is a necessary thing to do if someone is sick. Even if a friend or family member says they feel well enough to participate, you should wait until they are fully recovered and no longer contagious before spending time with that person.
Don't go to anyone's house if someone who lives there is sick, even if the sick person won't be present. Simply touching a doorknob or sitting on a couch with the sick person's germs can be enough to make you ill, especially if you have a compromised immune system because of COPD.
You should also be particularly careful when spending time in doctor's offices or hospitals, which carry an elevated risk of exposure to viruses and bacteria. Do your best to touch as few things as possible, and don't use items that other patients or people in the waiting room have touched.
Instead, anytime you have to go to the hospital or doctor's office, bring your own pen to sign yourself in. It's also a good idea to keep a small bottle of hand sanitizer with you anytime you go out in public to use after you touch doorknobs or other common surfaces.
Avoid Crowded Places

Large events and crowds are breeding pools for all kinds of viruses and bacteria. Even healthy people have to be extra cautious in large crowds and take extra precautions not to get sick.
But if you have COPD, you have to even more careful. Because COPD suppresses your immune system, people with the disease are much more prone to getting sick when exposed to lots of people's germs.
There's only so much you can do to protect yourself at large events with lots of people, which is why most doctors recommend avoiding large crowds altogether. It's just not worth taking the risk when getting sick could cause an exacerbation that could permanently damage your lungs or even be deadly.
Stay on Top of Your Medications

Even if you follow all of the advice above, you're likely to get sick if you don't keep up with your medications. It's important to take all the medications recommended by your doctor as prescribed to keep your lungs and airways healthy and resistant to disease.
If your doctor prescribes you antibiotics for a flare-up or exacerbation, always finish the entire course. Never stop taking them because you feel better, or you could end up with a serious antibiotic-resistant infection.
It's also important to use your bronchodilator medications to keep your airways open and clear. You should also practice mucus clearance techniques to get rid of excess mucus, which tends to trap bacteria and raise your chances for flare-ups and infections.
If you use supplemental oxygen, make sure you always have it around when you need it, especially during a flare-up or exacerbation. Using your supplemental oxygen helps you control breathlessness and other symptoms and prevent more serious complications and hospitalization.

Here are some additional tips for keeping up with your medications:
- Take your medications exactly as prescribed or recommended by your doctor.
- Try to take your medications at the exact time every day to make the habit easier to learn.
- Keep a calendar or schedule with all your medications listed along with how often you should take them.
- Set alarms on your phone to remind you to take your medication.
- Organize your medication every week into a pill box to save time and hassle.
- Talk to your doctor about what you should do if you miss a dose of medication. If you are late taking a dose, it's usually okay to take it as soon as you remember, unless you are supposed to be taking your next dose of the same medication very soon.
- Always get your new prescription before your current one runs out. It's best to get it filled at least a few days before you take your last dose of the previous batch so you have some wiggle room if there's any delay. Never wait until you've already run out of your medication to get or fill a new prescription!
- Always talk to your doctor before taking any supplements or over-the-counter medications. Anything that your doctor hasn't recommended could be unsafe for your condition or could interact with other prescription medications you are taking.
Wash Your Hands Often

Washing your hands is one of the best ways to avoid exposing yourself to germs that could get you sick, especially in public places where the risk of encountering a contagious virus or infection is much higher.
Bacteria and viruses get transferred to your hands whenever you touch common surfaces like grocery carts, doorknobs, pens, credit card readers, etc. If you don't clean your hands afterward, you can transfer these illness-causing germs directly to your body if you touch your eyes, nose, or mouth.
That's why you should wash your hands immediately after visiting any public place, including the library, grocery store, or gas station. You can also bring along a pocket container of hand sanitizer to use after touching surfaces that other people touch.
In-between hand-washings, make sure you don't inoculate yourself by making a special effort not to touch your face. If you follow these simple steps and avoid large crowds, you can significantly reduce your chances of contracting an illness from public places.
But first, you should make sure you know how to wash your hands the right way. Even though most people wash their hands daily, many don't know the proper and effective way to do it.
This is how you practice proper hand-washing technique:
- Wet: Start by wetting your hands under the faucet.
- Soap: Turn off the water and apply soap to your hands. (You can use liquid soap, powdered soap, or bar soap.)
- Lather: Next, rub your hands together with the soap to make it lather.
- Scrub: Spend about twenty seconds scrubbing your hands all over. Rub the soap all over every part of your hands, including the backs of your hands, wrists, palms, and in-between your fingers. If you need help timing it, you can hum the tune to “Happy Birthday” twice in your head to equal about twenty seconds. Don't forget to scrub underneath your fingernails, too (you can get a nail brush to keep by your sink to be more thorough).
- Rinse: Once you're done scrubbing, turn on the faucet and rinse your hands clean under the running water.
- Dry: Finally, get a clean towel to dry off your hands.
When to Wash Your Hands

You should be washing your hands and paying extra attention to hygiene all the time, not just when you're out in public. Even in your own home, you can greatly reduce your risk of getting sick by washing your hands on a regular basis.
Here's some general hand-washing tips you can use both at home and when you're out and about. We've split it into two sections, things you should wash your hands before doing and things you should wash your hands after.
Always Wash Your Hands Before:
- Preparing food (and during, as well, especially if you are handling meat)
- Eating a meal or snack
- Being around a sick or injured person
- Treating minor wounds and injuries
- Touching your face, nose, mouth, or eyes
Always Wash Your Hands After:
- Preparing food (especially after handling meat)
- Being around a sick or injured person
- Treating a wound or injury
- Touching an animal or pet
- Touching your pet's waste, toys, leash, or other items
- Using the bathroom
- Using chemicals or cleaners
- Using garden or lawn chemicals
- Shaking hands or touching another person
- Coughing, sneezing, or blowing your nose
- Touching garbage or handling trash
- Changing a diaper
- Being out in a public place
Stay Hydrated

Water is a vital and often underestimated tool for good health. Proper hydration gives you energy, boosts your immune system, and keeps your body working efficiently.
If you have COPD, drinking enough water is particularly important to keep your lungs and the rest of your body strong. It supports healthy muscles for better exercise, healthy digestion, and helps keep your airways clear and free from harmful bacteria.
When you get dehydrated, the mucus in your airways gets thicker, which blocks your airways and makes it more difficult to breathe. Thick mucus also traps bacteria and significantly increases your risk for respiratory illnesses and infections.
When you stay hydrated, your mucus is thinner and easier to clear out of your lungs and airways. It also reduces bloating, lubricates your respiratory tract, and keeps your immune system working efficiently.
Tips for Drinking Enough Water
Most adults should drink about six to eight cups of water each day, but it varies from person to person according to the CDC. You should drink water whenever you are thirsty and make an effort to hydrate multiple times throughout the day.
Stress, breathing difficulties, and mobility issues make it difficult for some people with COPD to drink enough water every day. Some people simply forget and don't drink water until they are already dehydrated.
Drinking soda, sugary juices, and other caffeinated beverages is another bad habit that can lead to dehydration. It's important to drink pure, fresh water whenever possible and limit how many sugary, carbonated, and alcoholic drinks you have.

Here are some general tips for staying hydrated with COPD:
- Many people with COPD tend to feel boated and experience breathing difficulties when their stomach is full, causing them to avoid eating or drinking. If this happens to you, try sipping or drinking small amounts of water at a time and spread it out through the day so it doesn't cause bloating and breathlessness. You might also avoid drinking water before meals so you save room for more calorie-dense foods and avoid getting too full.
- Avoid caffeinated, sugary, and sodium-filled drinks like sodas, fruit juice, and energy drinks. Caffeinated beverages can cause bloating and difficulty breathing, while sugary drinks are unhealthy and full of empty calories.
- Keep filled-up water bottles in strategic places around your house so you don't forget to hydrate and you always have a convenient source of water nearby.
- Always plan to drink extra water during the summer and when you do any physical activity. You have a much greater risk of dehydration whenever you exercise, sweat, or spend time in the heat.
- If you really want to drink something besides water, try milk, fruit-infused water, decaffeinated coffee, or decaffeinated tea. These are much better choices than sugary sodas or juices.
Get Better Sleep

Did you know that the quality of your sleep can have a huge effect on your COPD? Studies show that patients who get poor sleep are anywhere from ten to fifty percent more likely to experience an exacerbation.
Unfortunately, living with COPD makes getting enough sleep difficult for a variety of reasons. Sleep disorders are very common among people with COPD, and the disease comes with uncomfortable symptoms that can affect your quality of sleep.
Chest discomfort, difficulty breathing, and coughing are all extremely common COPD symptoms and, for some people, they get even worse at night. Dealing with these symptoms at bedtime makes getting to sleep and staying asleep extremely difficult.
Fortunately, there are several things you can do to get better quality sleep with COPD. By optimizing your sleeping environment, managing your symptoms, and taking care of any co-occurring sleep disorders you can get better rest and reduce your chances of having an acute exacerbation.

Here are some general tips for getting better sleep with COPD:
- Regular exercise and living an active lifestyle makes it easier to feel tired and fall asleep at night.
- Create a dark, cool, comfortable environment to sleep in. Make sure you have enough blankets to keep yourself at a comfortable temperature.
- If noises tend to wake you up at night or in the early morning, wear earplugs or use a white noise machine to block out disruptive sounds while you sleep.
- It is best to sleep on your back or your side for proper posture. Place a pillow or rolled up towel under your knees (if you lie on your back) or between your legs (if you lie on your side).
- Only use your bed for sleeping and sex, but nothing else. Don't keep your phone, laptop, tablet, or any other electronic device in or near your bed.
- Go to sleep and wake up at the same time every day, even on the weekends. This will help your body get on a regular schedule and make it easier to fall asleep.
- Avoid taking long naps or sleeping in too late; both can make it more difficult to get to sleep that night.
- If you suffer from acid reflux, which is particularly common among COPD patients, it can make it difficult to breathe at night. Avoid discomfort and breathing difficulties by eating a GERD-friendly diet and avoid eating food in the two to three hours before you go to bed.
- Avoid drinking alcohol or caffeine in the evenings.
- Prop up your head and neck with pillows to elevate them and make it easier to breathe.
- If you find it difficult to breathe when you sleep, talk to your doctor about using nighttime supplemental oxygen.
- Talk to your doctor about any medication side effects that might be making it difficult for you to sleep. Your doctor can identify any potential culprits and adjust your medication or dosage accordingly. DO NOT change medications or dosages without consulting your doctor first.
- Get a sleep test to check for sleep apnea, which is a very common sleep disorder in COPD patients. It happens when your airways collapse and obstruct your breathing while you sleep, causing you to wake up frequently without consciously realizing it. If it turns out you do have sleep apnea, you can get a mouthpiece or positive expiratory pressure (PEP) device that can improve your quality of sleep.

Get a Fingertip Pulse Oximeter

One of the earliest warning signs of a COPD flare-up or exacerbation is a drop in blood oxygen levels. This can happen when illness or inflammation reduces your respiratory function and your lungs can't get enough oxygen to supply your body.
Patients often don' t notice that their blood oxygen levels have fallen until they get a headache or start to feel dizzy, faint, or breathless. Some patients don't get any symptoms or don't notice them as a sign of low oxygen levels, and don't get help until their condition gets much more severe.
If left untreated, low blood oxygen levels can be very dangerous and even cause serious complications including heart problems and death in severe cases. It can also be a warning sign of an oncoming exacerbation, which is why it's so important to be able to recognize low blood oxygen saturation and treat it promptly.
That's when a quick diagnostic tool like a pulse oximeter can come in handy and possibly even save your life. A pulse oximeter can accurately and instantly read your blood oxygen levels to warn you if they get dangerously low.
This is a great way to make sure that you're getting enough oxygen and to monitor your COPD on a daily basis. By tracking your blood oxygen saturation readings and testing yourself often you can gain a lot of valuable information that can help you manage and treat your disease.
How to Use a Pulse Oximeter

To use your personal pulse oximeter at home, all you have to do is clamp the small, clamshell-shaped device onto the tip of your finger. In moments the device will display a readout of your current blood oxygen saturation levels on the screen.
The best part about using a pulse oximeter is that there is no pricking or pinching or discomfort involved at all. It's completely non-invasive, comfortable, and and incredibly easy to use.
It works by simply shining an infrared light onto the top of your finger, where it shines through your skin and to the sensor underneath. The light passes through blood vessels in your finger, and the sensor can tell how much of your blood is oxygenated based on your pulse rate and how much of the light gets absorbed by oxygen-rich red blood cells.

The pulse oximeter then shows your blood oxygen saturation as a SpO2 value, or as a percentage of the maximum amount of oxygen your blood can hold. It's important to know how to interpret these values to understand what it means in terms of your COPD.
Here is how you interpret the readings:
- SpO2 of 95%-100%: Normal, healthy range.
- Sp02 of 90%-95%: Slightly low oxygen saturation. It is not healthy for your oxygen saturation to be this low for extended periods of time.
- SpO2 less than 90%: Very low oxygen saturation. You should use supplemental oxygen when your saturation levels fall below 90%.
Pulse oximeters are generally very accurate, but you might need to get it calibrated first. Sometimes the baseline for your readouts needs to be adjusted based on your skin type or other physiological characteristics.
Although pulse oximeters are generally very simple to use, you can talk to your doctor if you have questions or need help calibrating it at first. Your doctor can also show you how to interpret the data and how to get the most accurate readings possible.
You should also be aware of a few things that can cause skewed or inaccurate readouts, like very cold skin or certain colors of nail polish. Here is a list of things to watch out for that could affect the accuracy of your pulse oximeter readings:
- Irregular blood flow or heart rate
- Poor circulation
- Very cold hands
- Dark nail polish (especially blue and black)
- Extremely bright lights
- Some pulse oximeters need to be specially calibrated for darker skin tones
When to Use Your Pulse Oximeter
A pulse oximeters is a great investment that can help you better manage your COPD in many different ways. It can help you better understand your symptoms, keep your oxygen levels in a healthy range, and even prevent serious exacerbations.
You can use your personal pulse oximeter as much as you like to check your blood oxygen levels throughout the day. It's a great way to figure out what kinds of activities and environments affect your oxygen levels and when to use your supplemental oxygen, if your doctor prescribes it.

It's also a great way to get early warning if something goes seriously wrong. If you feel ill or experience a flare-up, your pulse oximeter readings can let you know when your oxygen saturation levels drop low enough to warrant immediate medical attention.
Pulse oximeters are light, cheap, and an indispensable tool for people with severe COPD or who experience frequent exacerbations. Having your own pulse oximeter at home would not only help you stay healthy and give you peace of mind, but it could also give you early warning of a serious complication and save your life.
Eat the Right Foods for Healthy Lungs

Did you know that the foods that you eat can affect your COPD symptoms and how easy it is to breathe? That's right; your diet is intimately tied with your lung function and can have a significant impact on your health with COPD.
Certain foods are more taxing on your respiratory system and make your lungs have to work harder to absorb enough oxygen. Other foods are necessary for getting the right amounts of calories and nutrients, as well as preventing COPD-related weight loss and malnutrition.
If you eat unhealthy or inflammatory foods, have a low BMI, or don't get enough vitamins and minerals, you can significantly increase your chances for a COPD flare-up or exacerbation. When your lungs have to work harder or don't have the energy and nutrients they need to work efficiently, they are much more susceptible to triggers, irritants, and illnesses that can make your COPD symptoms significantly worse.
Foods to Avoid

There are certain foods, like processed meats and sugar that are unhealthy and may lead to inflammation that affects your ability to breathe. Other foods, like spicy and acidic foods, can cause bloating and stomach discomfort, especially if you have Gastroesophageal Reflux Disease (GERD).
Here are some examples of foods you should avoid in order to stay healthy and reduce your chances of having an exacerbation.

Foods that Cause Heartburn and Indegestion
- Very fatty and greasy foods
- Acidic foods
- Alcohol
- Garlic and onions
- Spicy foods and black pepper
- Tomatoes
- Citrusy fruits like lemons, oranges, and grapefruits
- Peppermint
- Cruciferous veggies (these tend to cause gas and bloating)
- Bonus Tip: Eat smaller meals throughout the day instead of three large ones, eat more slowly, and don't eat too close to bedtime to avoid heartburn and indigestion.

Sugary Foods
- Corn syrup
- Soda and fruit juices
- Pasta sauces
- Barbecue sauces
- Breakfast cereals
- Sweetened dairy products (flavored milk, yogurt, and cheeses)
- Low-fat foods (these tend to have extra sugar and salt added to make up for the bland taste caused by the reduced fat content)
- Always check the ingredient list on any packaged foods before you buy them to check for added sugars and salt. You will be surprised at how much extra sugar is packed into foods that you would never have guessed.

- Canned vegetables, soups, sauces, and salsas
- Pickled vegetables like pickles, pickled artichoke hearts, and olives
- Cured and processed meats
- Pizza
- Cheese
- Soda and energy drinks
- Bagels and other baked goods
- Condiments (e.g. ketchup and mustard)
- Frozen meals
- Instant noodle meals
- Processed, packaged snacks like crackers, chips, and pretzels

- Deli meats
- Cured meats
- Beef jerky
- Bacon
- Sausage
- Hot dogs
- Corned beef
- Canned meats and meat sauces
Foods You Should Eat

It's important to eat right in order to get enough nutrients to fuel your body and maintain a healthy BMI. Being underweight, overweight, or malnourished is a sure way to make your disease worse and increase your risk for exacerbations.
Now that you know what not to eat, you should know what kinds of fruits, veggies, proteins, and grains you should eat for a healthy and balanced diet. Getting enough calories is important, but getting them from the right sources is just as important to keep your lungs and the rest of your body strong.
Complex Carbohydrates

Every person needs a good balance of the three main macro nutrients in your diet: proteins, carbohydrates, and fats. If you have COPD, you need a slightly different balance of these nutrients in order to protect your lungs and minimize your respiratory symptoms.
In particular, COPD patients should eat fewer carbohydrates than what's usually recommended for healthy adults and eat more proteins and fats instead. That's because carbohydrates actually have a direct negative effect on your lungs.
The more carbohydrates you eat, the harder your lungs have to work in order absorb oxygen. Studies show that when people with COPD reduce their carbohydrate intake, it can cause noticeable improvements in lung function, reduce shortness of breath, and may even reduce the frequency of COPD exacerbations.
However, you still need to include healthy carbohydrates in your meals in order to get essential nutrients and provide your body with the energy it needs to function. Carbs are your body's most useful, immediate source of energy, and not getting enough can make you feel weak and fatigued.
Some carbs are much better than others, however, and you should always eat complex carbohydrates instead of simple carbs. Simple carbs cause spikes in blood sugar and are little more than empty calories, while complex carbohydrates give your body a longer-term source of energy.

Here are some examples of healthy carbohydrates you should include in your diet:
- Whole grain breads, crackers, and pastas
- Beans and peas
- Oats
- Popcorn
- Brown rice and wild rice
- High-fiber grains (e.g. barley, rye, and spelt)
- Starchy vegetables (e.g. potatoes, corn, pumpkin, and peas)
- Fresh, whole fruits with fiber
Lean Proteins

Muscle wasting is a common problem in people with COPD, which is why it's so important for people with the disease to get an adequate amount of protein their diet. Protein is vital for building and maintaining muscle, and if you don't get enough from your diet your body will break down your muscles to take their protein, instead.
This causes muscle weakness, fatigue, and makes exercising very difficult. And since exercise is one the most important parts of COPD treatment, it's very important to keep your muscles healthy and strong.
You should always seek out lean proteins instead of fatty proteins, and choose fresh, lean meats over processed meats. Seafood is fantastic source of protein and it usually contains moderate amounts of healthy omega-3 fatty acids.

Here are some examples of healthy proteins you should include in your diet:
- Fish (e.g. salmon, tuna, cod, bass, perch, halibut)
- Lean poultry (white meat chicken and white meat turkey)
- Dairy (milk, yogurt, and cheese)
- Lean beef
- Pork tenderloin
- Eggs
- Beans and legumes
- Soy (e.g. soymilk or tofu)
- Protein drinks and powders
Healthy Fats

Healthy fats are a very important part of a healthy diet for COPD. Fatty foods tend to be more calorie-dense which is great for patients on a high-calorie diet.
When you have COPD, your lungs have to work harder and use more energy, which means you need extra calories to make up the difference. If you are underweight or have difficulty getting enough calories, then adding more healthy fats to your diet is a great way to gain or maintain weight.
Not all fats are equally healthy, however. Nutritional guidelines say you should avoid trans fats and saturated fats when possible and choose unsaturated fats instead.
It's usually easy to tell the difference: saturated fats are solid at room temperature, while unsaturated fats are liquid. That means that vegetable oils are unsaturated, while butter is a saturated fat.

Here are some examples of healthy fats you should include in your diet:
- Vegetable oils, nut oils, and seed oils (e.g. olive oil, coconut oil, sunflower oil, and peanut oil)
- Fatty fish (e.g. salmon, anchovies, sardines, trout, Pacific and Atlantic mackerel, and herring) Plus, they have the added bonus of lots of heart-healthy omega-3 fatty acids.
- Nuts and nut butters (e.g. walnuts, almond butter, and macadamia nuts)
- Avocados
- Chia seeds
- Soybeans
- Dairy (milk, yogurt, and cheese)
- Eggs
- Dark chocolate
Vitamin D

Vitamin D is an important nutrient for a variety of reasons; it's necessary for healthy bones, calcium absorption, and a healthy immune system. Studies also show that vitamin D can prevent COPD exacerbations and even slow the pace at which patients lose lung function over time.
This is probably because, for a variety of reasons, COPD patients tend to be deficient in vitamin D. Researchers suspect that this deficiency leads to worsened symptoms and quicker disease progression, especially in people with advanced COPD.
Along with preventing exacerbations, vitamin D can help patients deficient in the vitamin recover from infections and exacerbations more quickly. Vitamin D is also important for the vital role it plays in repairing and maintaining your bones; COPD patients are particularly prone to bone weakness and osteoporosis, making it all the more necessary to get enough vitamin D in your diet.
Signs of Vitamin D Deficiency
Vitamin D deficiency usually results from an inadequate diet and too much time spent indoors. It tends to occur in people with COPD who are underweight and have difficulty eating enough food.
But diet alone is usually not enough to get an adequate amount of vitamin D every day. The rest usually comes from sunlight, which stimulates your body to produce vitamin D when it shines on your skin. Unfortunately, many vitamin D-deficient COPD patients are sedentary and spend hardly any time at all doing outdoor activities.
Vitamin D deficiency doesn't usually come with many symptoms, which is why most people who are deficient don't even realize it. However, there are some subtle signs of vitamin D deficiency that you should know how to recognize:
- Frequent illnesses or infections
- Wounds that take longer to heal
- Worsened fatigue
- Pain in bones
- Bone weakness
- Back pain
- Depression
How to Get Enough Vitamin D
If you have COPD, it's important to make sure your diet includes enough vitamin D. It will not only keep your bones and immune system strong, but it can even lower your risk of experiencing moderate or life-threatening exacerbations.

Most people should get about 1,000 IUs of vitamin D every day. Here are some foods you can eat to get more vitamin D in your diet:
- Tuna
- Swordfish
- Sake salmon
- Sardines
- Cod liver oil
- Beef liver
- Egg yolks
- Milk, yogurt, and other dairy products that are fortified with Vitamin D
- Orange juice fortified with vitamin D
- Vitamin D supplements
To up your vitamin D intake, try drinking vitamin-D-fortified orange juice with breakfast and eating fortified yogurt or cheese with a meal every day. You should also try to eat a vitamin D-rich fish like tuna or sake salmon once or twice a week.
It's also important to know that if you smoke, it actually reduces your body's ability to absorb vitamin D. Along with the fact that smoking damages your lungs, reduces your lifespan, and speeds up the progression of COPD, vitamin D deficiency is just one more thing to add to list of reasons why it's so important to quit smoking.
As final tip for getting extra vitamin D, spend a few minutes in the sun! Approximately ten minutes or so with the sun on your skin will give you about 1,000 IU of vitamin D. If you have dark pigmented skin, it will take longer. Don't forget to wear sunscreen the rest of the time, though; there's no need to damage your skin or increase your risk of cancer.
Get Plenty of Exercise
If you have COPD, physical activity should be your number one priority. It's the most effective way to strengthen your breathing muscles, improve your mobility, and improve your quality of life.
COPD patients who get more physical activity are stronger, healthier, and show fewer symptoms of anxiety and depression. Avoiding exercise and living a sedentary life, on the other hand, causes you to lose lung function quicker and experience an overall quicker physical decline.
That's why it's so very, incredibly important to be as active as you can every day. That can include daily walks around your neighborhood, weekly trips to the gym, or even chores and activities around the house.
What's most important is finding activities that you enjoy and that are appropriate for your physical condition. Your doctor can help you put together a personalized exercise plan that matches your fitness level and will help you improve your strength and health.
There are a variety of types of exercise, and most of them can be done from the comfort of your own home if you choose. In the next sections, we'll give you some pointers for well-rounded exercise and direct you to a variety of instructional resources you can use to get started.
Cardiovascular Exercise

Cardiovascular exercise is a type of exercise that uses continuous movement to get your heart rate and breathing rate up. This helps strengthen your heart and the muscles in your chest that you use to breathe, reducing COPD symptoms like chest tightness and shortness of breath.
There are a variety of cardiovascular activities you can do at home, including walking, biking, and jogging. Here are some other ideas for cardiovascular activities you can do to improve your COPD:
- Swimming
- Skating
- Tennis
- Zumba
- Dancing
- Paying with pets or children
- Low-impact aerobics
- Bicycling
- Walking
- Hiking
- Jogging
- Jumping rope
- Stair climbing
- Cleaning the house (e.g. vacuuming, raking, gardening, etc.)
Strength Exercises

While many COPD patients have difficulty exercising because of breathlessness and other symptoms, muscle weakness is actually the most common reason that patients avoid exercise. This highlights the importance of doing muscle strengthening exercises to improve endurance, mobility, and make it easier to stay active.
Some strength training exercises require weights, but you can do many strength exercises that don't require any equipment at all. However, if you don't have a gym membership, you might consider investing in a small set of lightweight hand weights so you can work out your arms more efficiently.
When you do strength training exercises, it's important to spend time on a variety of different muscle groups. Most exercises are categorized as either upper-body exercises or lower-body exercises, and some people tend to alternate focusing on upper-body or lower-body exercises with each workout.
You can find a variety of strength training videos online, including YouTube, to help you get started. You can also find strength workout DVDs on Amazon, from video stores, or even at your local library.
Here are some great instructional websites you can visit to practice new strength training exercises:
- Eldergym's huge list of strength training exercises for seniors
- Dr. Mercola's strength training exercises for seniors with instructional videos
- Recommended strength training exercises with images demonstrating each technique from the National Institute on Aging
- This complete PDF guide to strength training for older adults from the CDC
Stretching

Stretching is an important part of warming up and cooling down when you exercise. You should take at least a few minutes to stretch before and after every single workout.
Doing this helps limber up your body and get it ready for activity, improving your flexibility and reducing your chances for sprains and other injuries. Stretching is also a great light exercise to do every day, especially if you tend to get stiff, sore, or have limited mobility.
You should take time every day to stretch out common problem areas like your back, shoulders, legs, and arms. Here are a couple of great resources with instructions and pictures for stretching exercises you can practice:
- Eldergym's list of 12 flexibility exercises with instructional videos for each technique
- Evelo's complete guide to stretching exercises for seniors with accompanying images to demonstrate each move
Breathing Exercises
Controlling your breathing is a vital part of managing COPD symptoms like coughing and shortness of breath. You have to be able to slow and steady your breaths in order to recover from bouts of breathlessness and breathe normally again.
The best way to do this is by practicing tried and true breathing exercises recommended for people with respiratory diseases. Everyone who has COPD should be familiar with the two most basic breathing exercises: pursed lips breathing and diaphragmic breathing.
If you have COPD, you should practice these techniques often, even when you're not experiencing any acute symptoms. This strengthens your breathing muscles and helps you remember how to breathe correctly in the heat of those moments when your symptoms act up.
To learn more about breathing exercises that can help your COPD, visit the American Lung Association's website for detailed instructional videos you can follow along with. You can also get detailed instructions on a variety of breathing exercises from this article on Healthline and this page on the Lung Institute's website.
Make a COPD Action Plan
Disease self-management is a vital part of staying healthy and treating your COPD. That means following your COPD treatment plan and knowing how and when to use your different medications.
Many COPD patients have multiple prescriptions and medications for managing their symptoms; these might include bronchodilators, corticosteroids, antibiotics, supplemental oxygen, and more. Some of these medications are prescribed to be taken on a schedule, while others are used as-needed to address symptoms, flare-ups, and exacerbations as they happen.
It can be confusing to remember which medications to take and how bad your symptoms should be before you take them. You might be unsure of what symptoms warrant a call to your doctor or at what point you should go to the emergency room for worsened symptoms.
That's why it's important to have a COPD Action Plan, an easy-to-reference chart that helps you figure out what to do and what medications to take based on how you feel. There are sample action plans available from the American Lung Association and Australian Lung Foundation websites to give you an idea of how they work.
You will have to work with your doctor to put together an action plan that's tailored to you and your unique condition. After all, symptom severity varies widely among people with COPD, and your action plan will have to account for the range of symptoms you experience on a typical day.
Having an action plan in place will give you peace of mind and a solid, written set of guidelines for exactly how to manage your symptoms. Doing this will help you keep your symptoms in check, respond appropriately to flare-ups, and can significantly reduce your chance of experiencing an exacerbation. Even if you get an exacerbation despite managing your symptoms properly, following an action plan can reduce the time it takes to recover from the exacerbation.
COPD action plans are generally separated into three main sections, with each section addressing a different level of symptom severity. Here's a quick overview of what a three-part COPD action plan looks like.
Green Zone
![]()
The green zone refers to your baseline, how you feel on a normal, typical day. This is when your symptoms are at their lowest level and you're not experiencing a flare-up or exacerbation. Hopefully, this is the plan that you will follow on the vast majority of days.
When to Follow the Green Zone Plan:
- You feel well enough to do your usual daily activities
- You are having a typical amount of mucus and sputum
- You have a healthy appetite
- You are sleeping normally
Example Actions to Take in the Green Zone (your doctor will tailor this to your condition and medications):
- Take your daily medications as usual
- Follow your regular diet plan and exercise schedule
- Use supplemental oxygen (if prescribed) as usual
Yellow Zone
![]()
The yellow zone refers to days when your symptoms are acting up worse than usual. This might include days when you are experiencing a minor exacerbation or slightly worsened symptoms due to weather, allergies, or air pollution. You should follow your yellow-zone plan whenever your symptoms are elevated from their usual baseline.
When to Follow the Yellow Zone Plan:
- You have less energy for your usual daily activities
- You are experiencing increased or thickened mucus and sputum
- Your appetite is less than usual
- You are coughing more than usual
- You are getting poor sleep or wake up often because of your symptoms
- You are having to use your quick-relief medications more often than normal
- Your usual medications are not helping as well as they usually do
Example Actions to Take in the Yellow Zone (your doctor will tailor this to your condition and medications):
- Continue taking daily medications as usual
- Continue using supplemental oxygen (if prescribed) normally
- Use your quick relief medication more often (your doctor might give you a specific increment, such as every 3-4 hours)
- Start taking an oral corticosteroid medication (your doctor might include this in your plan along with the specific dosage and how often you should take it)
- Start taking an antibiotic (your doctor might include this in your plan along with the specific dosage and how often you should take it)
- Use pursed-lips breathing technique
- Try to get extra rest
- If your symptoms don't improve within a certain period of time (determined by your doctor), you should call your doctor right away.
Red Zone
![]()
The red zone is reserved for times when your symptoms become very severe, to the point that you need immediate medical attention. Being in the red zone is a medical emergency, and you doctor will tell you how to recognize when your symptoms get to that point.
When to Follow the Red Zone Plan:
- You are unable to do regular activities because of breathlessness
- You experience severe shortness of breath, even when resting
- Breathing difficulties are making it impossible to sleep
- You experience shaking, chills, or a fever
- You feel extremely drowsy, fatigued, or confused
- You are experiencing chest pains
- You are coughing up blood
Example Actions to Take in the Red Zone (your doctor will tailor this to your condition and medications):
- Call 911 or have someone take you to an emergency room right away
- While awaiting help from medical specialists, do the following: (your doctor will tell you the appropriate actions to take while you wait for professional care)
Conclusion
If you have COPD, then you know that periods of worsened symptoms are inevitable. However, the choices you make can have a significant influence on the frequency and severity of flare-ups and exacerbations.
But if you follow the steps in this article you can significantly reduce your risk for exacerbations and improve your chances for a full recovery if it happens. You just have to protect your lungs, take care of your body, and follow your COPD treatment plan along with any other advice your doctor gives you.
You can't always control or prevent an exacerbation, but you can control whether or not you make healthy choices. Now that you know a variety of ways to prevent COPD exacerbations, it's up to you to build the habits that will keep you healthy and strong.


.png)





